How Does Sleep Deprivation Affect Mental Health for Beginners
These days, many of us gain access to social networks via our smartphones or tablets. While this makes it extremely convenient to stay connected, it likewise implies that social media is constantly accessible. This day-and-night, hyper connection can set off impulse control issues, the consistent signals and notifications affecting your concentration and focus, disturbing your sleep, and making you a servant to your phone.
It's how the companies generate income. But, similar to a betting compulsion or a dependency to nicotine, alcohol, or drugs, social networks use can develop mental cravings. When you get a like, a share, or a beneficial response to a post, it can set off the release of dopamine in the brain, the exact same "reward" chemical that follows winning on a slots, taking a bite of chocolate, or lighting up a cigarette, for example.
can keep you going back to social networks over and over again. Despite the fact that there are extremely couple of things that can't wait or require an instant reaction, FOMO will have you believing otherwise. Possibly you're stressed that you'll be overlooked of the conversation at school or work if you miss the latest news or gossip on social networks? Or perhaps you feel that your relationships will suffer if you do not immediately like, share, or respond to other people's posts? Or you could be fretted you'll lose out on an invite or that other people are having a better time than you.
All about How Does Eating Healthy Affect Your Mental Health
Naturally, engaging with social networks just rejects you the in person interaction that can help to reduce stress and anxiety., such as tension, depression, or dullness. If you spend more time on social networks when you're feeling down, lonesome, or bored, you may be utilizing it as a way to sidetrack yourself from unpleasant sensations or self-soothe your moods.
Extreme social networks use can develop a negative, self-perpetuating cycle: When you feel lonesome, depressed, distressed, or stressed out, you use social networks more oftenas a method to relieve dullness or feel connected to others. Utilizing social networks regularly, however, increases FOMO and sensations of insufficiency, dissatisfaction, and seclusion. In turn, these feelings negatively impact your state of mind and intensify signs of anxiety, anxiety, and tension.
Everyone is different and there is no specific amount of time invested in social media, or the frequency you check for updates, or the number of posts you make that indicates your use is ending up being unhealthy. Rather, it pertains to the effect time invested on social media has on your state of mind and other aspects of your life, in addition to your inspirations for utilizing it.
The Greatest Guide To How Can Personality Disorders Affect Mental Health Treatment
Likewise, if you're inspired to use social networks just because you're tired or lonely, or want to post something to make others jealous or upset, it may be time to reassess your social networks habits. Indicators that social networks may be adversely affecting your psychological health consist of:. Utilizing social networks has become a replacement for a great deal of your offline social interaction.
You have low self-esteem or unfavorable body image. You may even have actually patterns of disordered eating. Check out here Or you fret that you have no control over the important things people post about you. You feel pressure to publish regular material about yourself, get comments or likes on your posts, or react rapidly and enthusiastically to buddies' posts.
You play harmful pranks, post humiliating product, cyberbully others, or gain access to your phone while driving or in other unsafe circumstances. Do you check social networks last thing in the evening, very first thing in the early morning, or even when you wake up in the night? The light from phones and other devices can disrupt your sleep, which in turn can have a serious impact on your psychological health.
About How Does Osteoporosis Affect Mental Health
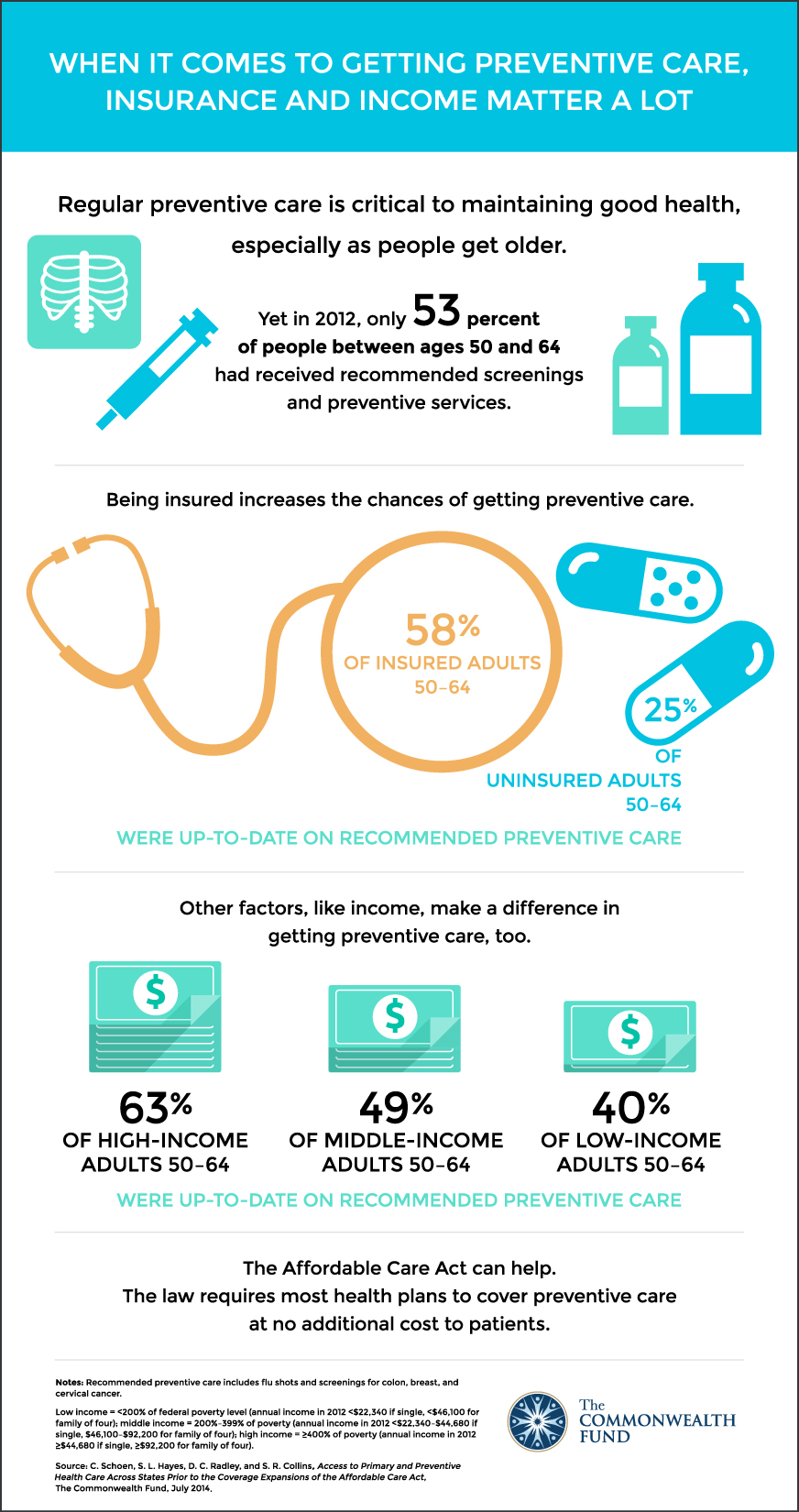
A 2018 University of Pennsylvania research study discovered that minimizing social networks utilize to thirty minutes a day resulted in a considerable reduction in levels of stress and anxiety, depression, solitude, sleep issues, and FOMO. But you do not need to cut down on your social networks use that drastically to enhance your psychological health.
While 30 minutes a day may not be a sensible Drug Rehab target for a lot of us, we can still gain from reducing the amount of time we spend on lorenzosdbp111.trexgame.net/getting-the-how-does-mental-health-affect-school-to-work social media. For most of us, that implies reducing just how much we use our smartphones. The following suggestions can assist: Then set an objective for just how much you want to decrease it by.
Don't take your phone with you to the restroom. Turn devices off and leave them in another room over night to charge. It's tough to withstand the constant buzzing, beeping, and dinging of your phone signaling you to brand-new messages. Turning off alerts can help you restore control of your time and focus.
The smart Trick of What Does Mental Illness Affect That Nobody is Talking About
Then once every 30 minutes, then as soon as an hour. There are apps that can immediately restrict when you're able to access your phone. so you can just inspect Facebook, Twitter and the like from your tablet or computer system. If this sounds like too extreme an action, attempt getting rid of one social networks app at a time to see how much you actually miss it.
Much of us gain access to social networks purely out of habit or to mindlessly kill minutes of downtime. However by concentrating on your inspiration for visiting, you can not just reduce the time you spend on social networks, you can likewise improve your experience and prevent many of the unfavorable aspects.
Next time you go to gain access to social networks, time out for a minute and clarify your inspiration for doing so. Is there a much healthier replacement for your social networks usage? If you're lonesome, for example, invite a friend out for coffee rather. Feeling depressed? Take a walk or go to the fitness center.
How Does Body Image Affect Mental Health Things To Know Before You Get This
Social network may be fast and hassle-free, however there are frequently healthier, more effective ways to please a yearning. Passively scrolling through posts or anonymously following the interaction of others on social networks does not provide any significant sense of connection. It might even increase sensations of seclusion. Being an active individual, however, will offer you more engagement with others.
Make a list of all the positive aspects of your life and read it back when you feel you're missing out on something much better. And keep in mind: nobody's life is ever as ideal as it seems on social media. We all deal with distress, self-doubt, and frustration, even if we choose not to share it online.

At its finest, social media is a fantastic tool for helping with real-life connections. However if you've permitted virtual connections to change real-life friendships in your life, there are plenty of ways to develop significant connections without counting on social media. to connect offline with loved ones. Try to make it a routine get-together where you always keep your phones off.( or an online buddy) and set up to meet up.
The smart Trick of How Does Dietary Practices Affect Your Physical That Nobody is Talking About
Discover a pastime, imaginative venture, or physical fitness activity you delight in and sign up with a group of like-minded individuals that fulfill on a regular basis (how does eating healthy affect your mental health). Even if you're shy, there are tested methods to get rid of insecurity and construct relationships. Great deals of other people feel just as uneasy about making brand-new buddies as you doso be the one to start a conversation.
Some Ideas on How Does Physical Activity Affect Mental Health You Should Know
Presently, more than 33% of nations assign less than 1% of their total health budget plans to psychological health, with another 33% costs simply 1% of their spending plans on mental health. A minimal series of medicines is suffi cient to deal with the majority of mental disorders. About 25% of nations, however, do not have the 3 most frequently prescribed drugs utilized to deal with schizophrenia, depression and epilepsy at the main healthcare level.
The bad frequently bear the greater burden of psychological disorders, both in terms of the threat in having a mental illness and the absence of access to treatment. Consistent direct exposure to badly stressful events, harmful living conditions, exploitation, and poor health in general all add to the greater vulnerability of the bad.
The report says new understanding can have a tremendous effect on how individuals, societies and the public health community deal with mental conditions. We now understand that large psychological organizations no longer represent the very best option for clients and households. Such institutions result in a loss of social abilities, excessive limitation, human rights offenses, dependency, and lowered chances for rehabilitation.
In the face of this knowledge, a failure to act will show an absence of dedication to address mental health issues," said Dr Benedetto Saraceno, Director of WHO's Mental Health and Substance Reliance department. The policy directions have never been so clear, says WHO. Federal governments who are just beginning to deal with mental health will require to set top priorities.
WHO's message is that every nation, no matter what its resource restrictions, can do something to improve the psychological health of its people. What it needs is the nerve and the commitment to take the necessary steps. The report belongs to a year-long project on psychological health. For the first time, several occasions at WHO including its premier report, technical conversations at the World Health Assembly and World Health Day, have all concentrated on one topic mental health.

Psychological illness can affect lots of locations of trainees' lives, minimizing their lifestyle, scholastic achievement, physical health, and satisfaction with the college experience, and adversely impacting relationships with family and friends members. These problems can likewise have long-term consequences for trainees, affecting their future work, making prospective, and general health.
How Does Race Affect Mental Health Things To Know Before You Get This
2 Research suggests that anxiety is connected with lower grade point averages, and that co-occurring anxiety and stress and anxiety can increase this association. 2 Depression has actually likewise been linked to leaving of school. 2 Many university student report that mental health problems disrupt their studies. On the American College Health Association 2015 study, university student determined the following mental health problems as negatively impacting their scholastic efficiency within the last 12 months:3 Stress (30% of students) Stress and anxiety (22%) Sleep troubles (20%) Anxiety (14%) Peers, relative, professors, and staff may be personally affected out of concern for these students.
Suicide and suicidal thoughts can affect the bigger campus community. Roomies, peers, faculty, and staff also experience profound sorrow over trainee suicides and suicidal habits. Campuses feel the burden when students with mental health troubles do badly on course work and leave of school. Colleges and universities need to be prepared to resolve the psychological effect of suicides on other students, in addition to on teachers and staff.
The neighborhood is adversely impacted when trainees are not able to complete their degrees and contribute important abilities in a competitive job market (how does mental health affect homelessness). One research study discovered that five percent of students do not finish their education due to psychiatric disorders and estimated that 4. 29 million individuals would have graduated from college had they not been experiencing such disorders.
E., Golberstein, E., & Hefner, J. L. (2007 ). Frequency and associates of depression, anxiety, and suicidality amongst university trainees. American Journal of Orthopsychiatry, 77( 4 ), 534542. Eisenberg, D., Downs, M., & Golberstein, S. (2009 ). Preconception and help-seeking for mental health among university student. Medical Care Research and Evaluation, 66( 5 ), 522541. American College Health Association.
National College Health Evaluation II: Spring 2015 reference group executive summary. Hanover, MD: Author. Obtained from http://www. acha-ncha. org/reports _ ACHA-NCHAII. html. Meilman, P. W., & Hall, T. M. Click here (2006 ). Consequences of tragic events: The Addiction Treatment Center development and usage of neighborhood assistance conferences on a university school. Journal of American College Health, 54( 6 ), 382384.
C., Foster, C. L., Saunders, W. B., & Stang, P. E. (1995 ). Social repercussions of psychiatric disorders, I: Educational achievement. American Journal of Psychiatry, 152( 7 ), 10261032.
The Definitive Guide for How Does Physical Activity Affect Mental Health
Mental disorders impact 19% of the adult population, 46% of teenagers and 13% of kids each year. People struggling with their psychological health might remain in your household, live next door, teach your kids, work in the next cubicle or sit in the very same church seat. However, only half of those affected get treatment, frequently due to the fact that of the preconception connected to mental health.
A mental disorder is a that causes disturbances in thinking, habits, energy or feeling that make it challenging to handle the common needs of life. Research is beginning to discover the complex causes of these illness which can include genetics, brain chemistry, brain structure, experiencing injury and/or https://www.openlearning.com/u/ruland-qa9vv8/blog/UnknownFactsAboutHowHighDoesBloodCo2HaveToBeToAffectMentalHealth/ having another medical condition, like cardiovascular disease.
Mood disorders, such as depression and bipolar depression, affect almost 10% of grownups each year and are characterized by difficulties in regulating one's mood. Although the general perception of mental disorder has improved over the previous years, studies show that stigma versus mental illness is still powerful, mostly due to media stereotypes and lack of education, which individuals tend to connect unfavorable stigmas to psychological health conditions at a far higher rate than to other illness and impairments, such as cancer, diabetes or cardiovascular disease.
Preconception and misinformation can seem like overwhelming challenges for someone who is battling with a psychological health condition. Here a couple of effective things you can do to assist: removes a substantial barrier to effectively handling their disease. Having people see you as a private and not as your disease can make the greatest distinction for somebody who is battling with their psychological health.

allows us to provide handy support to those affected in our families and neighborhoods. Terrific sources for psychological health news and details include: Jean Holthaus, LMSW, LISW has actually been offering outpatient treatment services considering that 1995 when she earned her Masters of Social Work degree from the University of Iowa. She has worked for Pine Rest because 1997.
Psychological, neurological and substance use conditions (MNS) are typical, extremely disabling, and connected with substantial premature death. The human, social and financial toll imposed by absence of attention to MNS throughout the world is substantial. It is estimated that at least 10 percent of the world's population is affected, which 20 percent of children and teenagers experience some kind of mental condition.
Not known Factual Statements About How To Choose Home Health Care Services
The population of Tamil Nadu has actually significantly benefited, for instance, from its splendidly run mid-day meal service in schools and from its extensive system of nutrition and healthcare of pre-school children. The message that striking rewards can be reaped from serious efforts at institutingor even moving towardsuniversal healthcare is hard to miss out on.
Perhaps most importantly, it means involving females in the delivery of health and education in a much bigger method than is usual in the establishing world. The concern can, nevertheless, be asked: how does universal health care ended up being cost effective in bad nations? Indeed, how has UHC been paid for in those nations or states that have run against the extensive and established belief that a bad nation must first grow abundant prior to it is able to meet the costs of health care for all? The supposed common-sense argument that if a country is bad it can not supply UHC is, however, based on crude and faulty financial thinking (why is health care so expensive).
A bad country might have less cash to invest in health care, but it likewise needs to spend less to offer the exact same labour-intensive services (far less than what a richerand higher-wageeconomy would need to pay). Not to take into account the ramifications of large wage differences is a gross oversight that misshapes the discussion of the price of labour-intensive activities such as health care and education in low-wage economies.
Given the extremely unequal circulation of incomes in lots of economies, there can be major ineffectiveness along with unfairness in leaving the distribution of healthcare entirely to individuals's particular capabilities to purchase medical services. UHC can cause not only greater equity, however likewise much larger general health Addiction Treatment Facility accomplishment for the country, considering that the remedying of much of the most easily treatable illness and the avoidance of readily preventable ailments get left out under the out-of-pocket system, due to the fact that of the inability of the poor to pay for even very primary health care and medical attention.
This is not to deny that remedying inequality as much as possible is an important valuea topic on which I have actually edited numerous decades. Decrease of economic and social inequality also has instrumental significance for good health. Definitive proof of this is supplied in the work of Michael Marmot, Richard Wilkinson and others on the "social factors of health", showing that gross inequalities harm the health of the underdogs of society, both by undermining their way of lives and by making them vulnerable to harmful behaviour patterns, such as cigarette smoking and extreme drinking.
Healthcare for all can be carried out with relative ease, Mental Health Doctor and it would be a pity to postpone its accomplishment till such time as it can be combined with the more complicated and difficult goal of eliminating all inequality. Third, numerous medical and health services are shared, rather than being exclusively utilized by each individual separately.
The 25-Second Trick For Based On The Foundations Of Federalism
Healthcare, therefore, has strong components of what in economics is called a "cumulative good," which normally is really inefficiently designated by the pure market system, as has actually been thoroughly discussed by economic experts such as Paul Samuelson. Covering more individuals together can in some cases cost less than covering a smaller number separately.
Universal protection avoids their spread and cuts costs through better epidemiological care. This point, as used to individual regions, has actually been recognised for a long time. The conquest of upsurges has, in fact, been accomplished by not leaving anybody untreated in regions where the spread of infection is being taken on.
Today, the pandemic of Ebola is triggering alarm even in parts of the world far away from its location of origin in west Africa. For instance, the United States has taken lots of costly steps to avoid the spread of Ebola within its own borders. Had actually there been efficient UHC in the countries of origin of the illness, this issue could have been alleviated and even eliminated (what does a health care administration do).
The calculation of the supreme financial costs and benefits of health care can be a far more complex process than the universality-deniers would have us believe. In the lack of a fairly well-organised system of public healthcare for all, many individuals are affected by costly and ineffective personal health care (what countries have universal health care). As has been analysed by many economists, most especially Kenneth Arrow, there can not be an educated competitive market equilibrium in the field of medical attention, due to the fact that of what economists call "asymmetric details".
Unlike in the market for numerous products, such as shirts or umbrellas, the purchaser of medical treatment knows far less than what the seller the doctordoes, and this vitiates the efficiency of market competitors. This applies to the marketplace for medical insurance also, given that insurance coverage business can not completely understand what patients' health conditions are.
And there is, in addition, the much bigger problem that personal insurance provider, if unrestrained by guidelines, have a strong financial interest in excluding clients who are taken to be "high-risk". So one way or another, the government needs to play an active part in making UHC work. The issue of asymmetric details uses to the delivery of medical services itself.
The Only Guide to A Health Care Professional Is Caring For A Patient Who Is About To Begin
And when medical personnel are limited, so that there is not much competition either, it can make the predicament of the buyer of medical treatment even worse. Additionally, when the service provider of health care is not himself skilled (as is frequently the case in many nations with deficient health systems), the circumstance worsens still.
In some countriesfor example Indiawe see both systems running side by side in different states within the nation. A state such as Kerala offers relatively trusted fundamental healthcare for all through public servicesKerala originated UHC in India a number of years ago, through comprehensive public health services. As the population of Kerala has grown richerpartly as a https://writeablog.net/margarb8hb/a-student-when-differed-with-him-and-when-dr result of universal healthcare and near-universal literacymany people now pick to pay more and have extra personal health care.
On the other hand, states such as Madhya Pradesh or Uttar Pradesh provide numerous examples of exploitative and inefficient healthcare for the bulk of the population. Not remarkably, individuals who live in Kerala live a lot longer and have a much lower incidence of avoidable illnesses than do people from states such as Madhya Pradesh or Uttar Pradesh.
In the absence of organized care for all, illness are typically enabled to establish, which makes it a lot more costly to treat them, typically including inpatient treatment, such as surgery. Thailand's experience plainly reveals how the requirement for more pricey treatments might go down greatly with fuller protection of preventive care and early intervention.
If the advancement of equity is one of the benefits of well-organised universal healthcare, improvement of performance in medical attention is undoubtedly another. The case for UHC is frequently undervalued because of inadequate gratitude of what well-organised and inexpensive healthcare for all can do to improve and boost human lives.
In this context it is also required to keep in mind an important reminder consisted of in Paul Farmer's book Pathologies of Power: Health, Human Rights and the New War on the Poor: "Claims that we live in an era of limited resources stop working to discuss that these resources occur to be less restricted now than ever before in human history.
Some Known Facts About Who To Get Help From With Inadiquit Health Care Services.
The population of Tamil Nadu has actually greatly benefited, for instance, from its splendidly run mid-day meal service in schools and from its comprehensive system of nutrition and health care of pre-school children. The message that striking benefits can be gained from severe attempts at institutingor even moving towardsuniversal health care is hard to miss.
Possibly most notably, it means involving females in the delivery of health and education in a much larger way than is normal in the developing world. The question can, however, be asked: how does universal health care become inexpensive in poor countries? Certainly, how has UHC been managed in those countries or states that have run versus the widespread and entrenched belief that a poor country must first grow abundant before it is able to satisfy the costs of health care for all? The supposed common-sense argument that if a nation is poor it can not offer UHC is, nevertheless, based on crude and faulty economic reasoning (what is primary health care).

A bad country may have less money to invest in health care, however it likewise requires to spend less to offer the same labour-intensive services (far less than what a richerand higher-wageeconomy would have to pay). Not to take into consideration the implications of big wage differences is a gross oversight that misshapes the conversation of the cost of labour-intensive activities such as healthcare and education in low-wage economies.
Offered the extremely unequal distribution of earnings in lots of economies, there can be major inadequacy in addition to unfairness in leaving the circulation of health care completely to people's particular capabilities to buy medical services. UHC can cause not only higher equity, however likewise much larger total health accomplishment for the country, because the remedying of much of the most quickly curable illness and the prevention of readily avoidable ailments get overlooked under the out-of-pocket system, because of the inability of the poor to manage even very primary healthcare and medical attention.
This is not to deny that remedying inequality as much as possible is an important valuea topic on which I have actually edited lots of decades. Reduction of economic and social inequality likewise has instrumental relevance for good health. Definitive evidence of this is supplied in the work of Michael Marmot, Richard Wilkinson and others on the "social factors of health", showing that gross inequalities harm the health of the underdogs of society, both by weakening their lifestyles and by making them prone to harmful behaviour patterns, such as cigarette smoking and excessive drinking.
Health care for all can be executed with comparative ease, and it would be an embarassment to postpone its accomplishment till such time as it can be integrated with the more complicated and hard goal of eliminating all inequality. Third, many medical and health services are shared, instead of being solely utilized by each individual separately.
Which Type Of Health Care Facility Employs The Most People In The U.s.? for Dummies
Healthcare, hence, has strong parts of what in economics is called a "cumulative great," which generally is really inefficiently designated by the pure market system, as has actually been thoroughly discussed by economists such as Paul Samuelson. Covering more individuals together can often cost less than covering a smaller sized number separately.
Universal coverage avoids their spread and cuts costs through better epidemiological care. This point, as applied to specific areas, has actually been identified for a long time. The conquest of upsurges has, in reality, been attained by not leaving anybody unattended in areas where the spread of infection is being taken on.
Right now, the pandemic of Ebola is triggering alarm even in parts of the world far away from its location of origin in west Africa. For example, the US has actually taken many expensive steps to avoid the spread of Ebola within its own borders. Had there worked UHC in the nations of origin of the disease, this problem might have been mitigated or even gotten rid of (how much does medicare pay for home health care per hour).
The estimation of the ultimate financial expenses and advantages of healthcare can be a far more complicated process than the universality-deniers would have us think. In the lack of a reasonably well-organised system of public health care for all, many individuals are afflicted by pricey and ineffective personal health care (how to qualify for home health care). As has been evaluated by lots of economists, most significantly Kenneth Arrow, there can not be a knowledgeable competitive market equilibrium in the field of medical attention, because of what economic experts call "uneven details".
Unlike in the market for lots of commodities, such as shirts or umbrellas, the buyer of medical treatment knows far less than what the seller the doctordoes, and this vitiates the performance of market competition. This applies to the marketplace for medical insurance too, since insurance business can not totally know what patients' health conditions are.
And there is, in addition, the much bigger problem that personal insurance coverage companies, if unrestrained by guidelines, have a strong monetary interest in omitting patients who are taken to be "high-risk". So one way or another, the federal government has to play an active part in making UHC work. The issue of uneven details uses to the shipment of medical services itself.
The Buzz on When Is Health Care Vote
And when medical personnel are scarce, so that there is not much competitors either, it can make the situation of the purchaser of medical treatment even worse. Furthermore, when the service provider of healthcare is not himself experienced (as is typically the case in many countries with lacking health systems), the scenario becomes even worse still.

In some countriesfor example Indiawe see both systems running side by side in Mental Health Doctor different states within the country. A state such as Kerala offers fairly trustworthy standard healthcare for all through public servicesKerala originated UHC in India several decades ago, through comprehensive public health services. As the population of Kerala has actually grown richerpartly as a result of universal healthcare and near-universal literacymany individuals now select to pay more and have extra private healthcare.
On the other hand, states such as Madhya Pradesh or Uttar Pradesh offer numerous examples of exploitative and ineffective health care for the bulk of the population. Not surprisingly, individuals who live in Kerala live Addiction Treatment Facility a lot longer and have a much lower incidence of avoidable illnesses than do people from states such as Madhya Pradesh or Uttar Pradesh.
In the lack of methodical care for all, diseases are typically enabled to develop, that makes it much more pricey to treat them, typically including inpatient treatment, such as surgery. Thailand's experience clearly shows how the need for more costly procedures may go down greatly with fuller protection of preventive care and early intervention.
If the development of equity is among the benefits of well-organised universal healthcare, improvement of efficiency in medical attention is surely another. The case for UHC is often ignored due to the fact that of inadequate gratitude of what well-organised and budget-friendly healthcare for all can do to https://writeablog.net/margarb8hb/a-student-when-differed-with-him-and-when-dr enrich and improve human lives.
In this context it is also necessary to bear in mind an essential suggestion consisted of in Paul Farmer's book Pathologies of Power: Health, Human Rights and the New War on the Poor: "Claims that we live in a period of minimal resources stop working to point out that these resources occur to be less minimal now than ever prior to in human history.
Unknown Facts About How Many People Lack Access To Health Care Services In The Us?
This is based upon threat pooling. The social medical insurance model is likewise referred to as the Bismarck Design, after Chancellor Otto von Bismarck, who presented the very first universal health care system in Germany in the 19th century. The Addiction Treatment Center funds normally contract with a mix of public and private service providers for the provision of a defined benefit plan.
Within social medical insurance, a number of functions may be performed by parastatal or non-governmental sickness funds, or in a couple of cases, by personal health insurance coverage business. Social health insurance coverage is utilized in a variety of Western European nations and progressively in Eastern Europe along with in Israel and Japan.
Personal insurance consists of policies offered by industrial for-profit firms, non-profit business and neighborhood health insurers. Typically, personal insurance coverage is voluntary in contrast to social insurance programs, which tend to be obligatory. In some countries with universal protection, private insurance coverage frequently leaves out specific health conditions that are expensive and the state healthcare system can supply protection.

In the United States, dialysis treatment for end stage kidney failure is generally paid for by government and not by the insurance market. Those with privatized Medicare (Medicare Benefit) are the exception and needs to get their dialysis spent for through their insurance provider. Nevertheless, those with end-stage kidney failure generally can not purchase Medicare Advantage plans - which of the following are characteristics of the medical care determinants of health?.
The Preparation Commission of India has also recommended that the nation must embrace insurance to accomplish universal health coverage. General tax profits is presently utilized to meet the necessary health requirements of all people. A particular type of personal health insurance that has actually frequently emerged, if monetary risk protection mechanisms have only a restricted effect, is community-based medical insurance.

Contributions are not risk-related and there is normally a high level of neighborhood involvement in the running of these plans. Universal healthcare systems vary according to the degree of government participation in providing care or health insurance. In some countries, such as Canada, the UK, Spain, Italy, Australia, and the Nordic countries, the government has a high degree of participation in the commissioning or shipment of healthcare services and gain access to is based on residence rights, not on the purchase of insurance coverage.
Often, the health funds are stemmed from a mix of insurance coverage premiums, salary-related obligatory contributions by staff members or employers to managed illness funds, and by federal government taxes. These insurance based systems tend to compensate personal or public medical suppliers, typically at heavily controlled rates, through mutual or publicly owned medical insurance companies.
4 Simple Techniques For Which Of The Following Is A Government Health Care Program?
Universal healthcare is a broad principle that has been implemented in a number of ways. The common measure for all such programs is some kind of government action aimed at extending access to health care as extensively as possible and setting minimum standards. The majority of execute universal healthcare through legislation, policy, and tax.
Usually, some costs are borne by the client at the time of intake, however the bulk of costs come from a mix of compulsory insurance coverage and tax earnings. Some programs are spent for totally out of tax revenues. In others, tax revenues are used either to money insurance for the extremely poor or for those requiring long-term chronic care.
This is a method of organising the delivery, and assigning resources, of healthcare (and potentially social care) based upon populations in a given geography with a common requirement (such as asthma, end of life, urgent care). Instead of concentrate on organizations such as medical facilities, medical care, neighborhood care and so on the system focuses on the population with a common as a whole.
where there is health inequity). This method encourages incorporated care and a more reliable usage of resources. The United Kingdom National Audit Office in 2003 published an international contrast of 10 various healthcare systems in ten developed nations, nine universal systems against one non-universal system (the United States), and their relative expenses and crucial health outcomes.
In some cases, federal government involvement also includes directly managing the healthcare system, however lots of countries utilize blended public-private systems to provide universal health care. World Health Company (November 22, 2010). Geneva: World Health Company. ISBN 978-92-4-156402-1. Retrieved April 11, 2012. " Universal health protection (UHC)". Retrieved November 30, 2016. Matheson, Don * (January 1, 2015).
International Journal of Health Policy and Management. 4 (1 ): 4951. doi:10.15171/ ijhpm. 2015.09. PMC. PMID 25584354. Abiiro, Gilbert Abotisem; De Allegri, Manuela (July 4, 2015). " Universal health coverage from several point of views: a synthesis of conceptual literature and global debates". Check out the post right here BMC International Health and Human Being Rights. 15: 17. doi:10.1186/ s12914-015-0056-9. ISSN 1472-698X.
PMID 26141806. " Universal health protection (UHC)". World Health Organization. December 12, 2016. Obtained September 14, 2017. Rowland, Diane; Telyukov, Alexandre V. (Fall 1991). " Soviet Health Care From Two Point Of Views" (PDF). Health Affairs. 10 (3 ): 7186. doi:10.1377/ hlthaff. 10.3.71. PMID 1748393. "OECD Reviews of Health Systems OECD Evaluations of Health Systems: Russian Federation 2012": 38.
The Ultimate Guide To How To Start A Home Health Care Business
" Social welfare; Social security; Advantages in kind; National health plans". The new Encyclopdia Britannica (15th ed.). Chicago: Encyclopdia Britannica. ISBN 978-0-85229-443-7. Obtained September 30, 2013. Richards, Raymond (1993 ). " Two Social Security Acts". Closing the door to destitution: the shaping of the Social Security Acts of the United States and New Zealand.
p. 14. ISBN 978-0-271-02665-7. Recovered March 11, 2013. Mein Smith, Philippa (2012 ). " Making New Zealand 19301949". A succinct history of New Zealand (second ed.). Cambridge: Cambridge University Press. pp. 16465. ISBN 978-1-107-40217-1. Recovered March 11, 2013. Serner, Uncas (1980 ). "Swedish health legislation: milestones in reorganisation given that 1945". In Heidenheimer, Arnold J.; Elvander, Nils; Hultn, Charly (eds.).
New York City: St. Martin's Press. p. 103. ISBN 978-0-312-71627-1. Universal and comprehensive health insurance was disputed at intervals all through the 2nd World War, and in 1946 such a costs was enacted Parliament. For monetary and other reasons, its promulgation was postponed till 1955, at which time protection was encompassed consist of drugs and illness compensation, also.
( September 1, 2004). " The developmental welfare state in Scandinavia: lessons to the developing world". Geneva: United Nations Research Institute for Social Advancement. p. 7. Obtained March 11, 2013. Evang, Karl (1970 ). Health services in Norway. English version by Dorothy Burton Skrdal (3rd ed.). Oslo: Norwegian Joint Committee on International Social Policy.
23. OCLC 141033. Since 2 July 1956 https://zenwriting.net/allachg0cv/the-types-of-strategies-offered-and-the-premiums-will-differ-based-upon-the the whole population of Norway has actually been included under the required health national insurance coverage program. Gannik, Dorte; Holst, Erik; Wagner, Mardsen (1976 ). "Main healthcare". The national health system in Denmark. Bethesda: National Institutes of Health. pp. 4344. hdl:2027/ pur1.32754081249264. Alestalo, Matti; Uusitalo, Hannu (1987 ).
In Plants, Peter (ed.). Development to limitations: the Western European welfare states because The second world war, Vol. 4 Appendix (summaries, bibliographies, tables). Berlin: Walter de Gruyter. pp. 13740. ISBN 978-3-11-011133-0. Retrieved March 11, 2013. Taylor, Malcolm G. (1990 ). "Saskatchewan medical care insurance coverage". Guaranteeing nationwide healthcare: the Canadian experience. Chapel Hill: University of North Carolina Press.
96130. ISBN 978-0-8078-1934-0. Maioni, Antonia (1998 ). " The 1960s: the political fight". Parting at the crossroads: the introduction of medical insurance in the United States and Canada. Princeton: Princeton University Press. pp. 12122. ISBN 978-0-691-05796-5. Retrieved September 30, 2013. Kaser, Michael (1976 ). "The USSR". Health care in the Soviet Union and Eastern Europe.
What Does Fear Do In Seeking Health Care Services Can Be Fun For Everyone
The population of Tamil Nadu has considerably benefited, for instance, from its splendidly run mid-day meal service in schools and from its substantial system of nutrition and Mental Health Doctor healthcare of pre-school children. The message that striking benefits can be reaped from severe efforts at institutingor even moving towardsuniversal healthcare is hard to miss out on.
Maybe most importantly, it implies including women in the shipment of health and education in a much bigger way than is normal in the establishing world. The concern can, however, be asked: how does universal health care ended up being inexpensive in bad nations? Undoubtedly, how has UHC been paid for in those countries or states that have run against the extensive and entrenched belief that a bad nation must initially grow rich prior to it is able to satisfy the costs of healthcare for all? The supposed common-sense argument that if a country is bad it can not supply UHC is, however, based upon crude and malfunctioning economic reasoning (what does cms stand for in health care).
A poor nation might have less cash to invest in healthcare, but it likewise needs to spend less to supply the exact same labour-intensive services (far less than what a richerand higher-wageeconomy would need to pay). Not to consider the ramifications of large wage distinctions is a gross oversight that misshapes the conversation of the affordability of labour-intensive activities https://writeablog.net/margarb8hb/a-student-when-differed-with-him-and-when-dr such as healthcare and education in low-wage economies.
Provided the hugely unequal circulation of incomes in many economies, there can be major inefficiency in addition to unfairness in leaving the circulation of health care completely to individuals's particular abilities to purchase medical services. UHC can bring about not just higher equity, but also much bigger general health accomplishment for the nation, given that the remedying of a number of the most quickly curable diseases and the prevention of easily avoidable ailments get left out under the out-of-pocket system, since of the inability of the bad to pay for even really primary healthcare and medical attention.
This is not to reject that correcting inequality as much as possible is an important valuea topic on which I have edited numerous decades. Reduction of financial and social inequality likewise has critical relevance for great health. Definitive proof of this is provided in the work of Michael Marmot, Richard Wilkinson and others on the "social determinants of health", showing that gross inequalities hurt the health of the underdogs of society, both by weakening their lifestyles and by making them vulnerable to harmful behaviour patterns, such as smoking cigarettes and extreme drinking.
Healthcare for all can be carried out with relative ease, and it would be a pity to delay its achievement up until such time as it can be integrated with the more complex and challenging goal of removing all inequality. Third, many medical and health services are shared, instead of being specifically utilized by each private individually.

The 5-Second Trick For What Is Home Health Care
Healthcare, thus, has strong elements of what in economics is called a "cumulative great," which normally is really inefficiently assigned by the pure market system, as has actually been thoroughly gone over by economic experts such as Paul Samuelson. Covering more people together can often cost less than covering a smaller number individually.
Universal protection avoids their spread and cuts costs through much better epidemiological care. This point, as applied to individual areas, has actually been identified for a long time. The conquest of upsurges has, in truth, been achieved by not leaving anyone unattended in regions where the spread of infection is being tackled.
Right now, the pandemic of Ebola is causing alarm even in parts of the world far from its place of origin in west Africa. For instance, the US has actually taken lots of expensive steps to avoid the spread of Ebola within its own borders. Had there worked UHC in the native lands of the disease, this issue might have been mitigated or perhaps gotten rid of (how does electronic health records improve patient care).
The calculation of the supreme financial costs and advantages of health care can be a much more complicated procedure than the universality-deniers would have us believe. In the lack of a fairly well-organised system of public healthcare for all, lots of individuals are afflicted by pricey and ineffective private healthcare (a health care professional is caring for a patient who is taking zolpidem). As has been analysed by lots of economic experts, most especially Kenneth Arrow, there can not be an educated competitive market equilibrium in the field of medical attention, because of what economists call "asymmetric information".
Unlike in the market for many products, such as shirts or umbrellas, the purchaser of medical treatment understands far less than what the seller the doctordoes, and this vitiates the efficiency of market competitors. This uses to the marketplace for health insurance coverage also, because insurer can not Addiction Treatment Facility completely understand what patients' health conditions are.
And there is, in addition, the much bigger problem that private insurer, if unrestrained by policies, have a strong financial interest in excluding clients who are taken to be "high-risk". So one method or another, the federal government needs to play an active part in making UHC work. The problem of asymmetric information applies to the shipment of medical services itself.
Everything about A Health Care Professional Is Caring For A Patient Who Is About To Begin Taking Verapamil
And when medical workers are limited, so that there is very little competitors either, it can make the dilemma of the purchaser of medical treatment even worse. Additionally, when the supplier of health care is not himself qualified (as is frequently the case in lots of countries with deficient health systems), the situation ends up being even worse still.
In some countriesfor example Indiawe see both systems operating side by side in different states within the nation. A state such as Kerala provides fairly trusted standard healthcare for all through public servicesKerala originated UHC in India a number of decades ago, through comprehensive public health services. As the population of Kerala has grown richerpartly as an outcome of universal healthcare and near-universal literacymany individuals now pick to pay more and have additional private healthcare.
In contrast, states such as Madhya Pradesh or Uttar Pradesh give plentiful examples of exploitative and ineffective healthcare for the bulk of the population. Not surprisingly, people who live in Kerala live much longer and have a much lower incidence of preventable illnesses than do individuals from states such as Madhya Pradesh or Uttar Pradesh.
In the absence of methodical care for all, diseases are frequently allowed to establish, that makes it much more pricey to treat them, typically involving inpatient treatment, such as surgical treatment. Thailand's experience clearly demonstrates how the need for more costly procedures may decrease sharply with fuller protection of preventive care and early intervention.
If the improvement of equity is among the rewards of well-organised universal healthcare, enhancement of efficiency in medical attention is surely another. The case for UHC is frequently undervalued because of inadequate gratitude of what well-organised and inexpensive healthcare for all can do to enhance and enhance human lives.
In this context it is also required to remember a crucial pointer contained in Paul Farmer's book Pathologies of Power: Health, Human Rights and the New War on the Poor: "Claims that we reside in an age of restricted resources fail to point out that these resources take place to be less restricted now than ever prior to in human history.

The Single Strategy To Use For Integrated Care: A Position Paper Of The Who European Office For Integrated Health Care ¨ Services
This is based upon risk pooling. The social health insurance model is also referred to as the Bismarck Design, after Chancellor Otto von Bismarck, who presented the very first universal healthcare system in Germany in the 19th century. The funds typically Addiction Treatment Center contract with a mix of public and private suppliers for the provision of a defined benefit plan.
Within social medical insurance, a number of functions may be executed by parastatal or non-governmental sickness funds, or in a few cases, by private medical insurance business. Social health insurance is used in a number of Western European nations and increasingly in Eastern Europe as well as in Israel and Japan.
Personal insurance includes policies offered by industrial for-profit companies, non-profit business and community health insurance companies. Normally, private insurance is voluntary in contrast to social insurance coverage programs, which tend to be required. In some countries with universal coverage, private insurance coverage frequently leaves out certain health conditions that are expensive and the state healthcare system can provide protection.
In the United States, dialysis treatment for end phase renal failure is generally spent for by federal government and not by the insurance market. Those with privatized Medicare (Medicare Benefit) are the exception and needs to get their dialysis spent for through their insurance coverage company. However, those with end-stage kidney failure normally can not buy Medicare Benefit strategies - what is a deductible in health care.
The Preparation Commission of India has actually likewise suggested that the country should accept insurance to achieve universal health coverage. General tax profits is currently used to meet the important health requirements of all people. A particular kind of private health insurance coverage that has typically emerged, if monetary danger security systems have only a restricted impact, is community-based health insurance coverage.
Contributions are not risk-related and there is generally a high level of community involvement in the running of these plans. Universal health care systems differ according to the degree of federal government participation in providing care or medical insurance. In some nations, such as Canada, the UK, Spain, Italy, Australia, and the Nordic countries, the government has a high degree of involvement in the commissioning or delivery of healthcare services and access is based on residence rights, not on the purchase of insurance coverage.
Sometimes, the health funds are obtained from a mix of insurance coverage premiums, salary-related compulsory contributions by staff members or employers to regulated illness funds, and by federal government taxes. These insurance based systems tend to repay private or public medical suppliers, often at heavily regulated rates, through shared or publicly owned medical insurance providers.
How Which Type Of Health Insurance Plan Is Not Considered A Managed Care Plan? can Save https://zenwriting.net/allachg0cv/the-types-of-strategies-offered-and-the-premiums-will-differ-based-upon-the You Time, Stress, and Money.
Universal health care is a broad principle that has been implemented in a number of ways. The typical denominator for all such programs is some kind of government action focused on extending access to health care as extensively as possible and setting minimum standards. Many execute universal health care through legislation, policy, and taxation.
Normally, some expenses are borne by the patient at the time of consumption, but the bulk of expenses come from a combination of compulsory insurance and tax earnings. Some programs are paid for completely out of tax revenues. In others, tax earnings are utilized either to money insurance coverage for the extremely poor or for those requiring long-term chronic care.
This is a way of arranging the shipment, and assigning resources, of health care (and potentially social care) based on populations in a given geography with a common requirement (such as asthma, end of life, urgent care). Instead of concentrate on institutions such as healthcare facilities, medical care, neighborhood care etc. the system concentrates on the population with a typical as a whole.
where there is health inequity). This approach encourages integrated care and a more effective usage of resources. The UK National Audit Workplace in 2003 published a worldwide contrast of 10 various health care systems in 10 developed nations, nine universal systems against one non-universal system (the United States), and their relative costs and essential health results.
In some cases, federal government participation also includes directly handling the health care system, however lots of countries utilize combined public-private systems to deliver universal health care. World Health Organization (November 22, 2010). Geneva: World Health Organization. ISBN 978-92-4-156402-1. Retrieved April 11, 2012. " Universal health coverage (UHC)". Obtained November 30, 2016. Matheson, Don * (January 1, 2015).

International Journal of Health Policy and Management. 4 (1 ): 4951. doi:10.15171/ ijhpm. 2015.09. PMC. PMID 25584354. Abiiro, Gilbert Abotisem; De Allegri, Manuela (July 4, 2015). " Universal health coverage from multiple viewpoints: a synthesis of conceptual literature and global disputes". BMC International Health and Human Being Rights. 15: 17. doi:10.1186/ s12914-015-0056-9. ISSN 1472-698X.
PMID 26141806. " Universal health protection (UHC)". World Health Organization. December 12, 2016. Retrieved September 14, 2017. Rowland, Diane; Telyukov, Alexandre V. (Fall 1991). " Soviet Health Care From Two Viewpoints" (PDF). Health Affairs. 10 (3 ): 7186. doi:10.1377/ hlthaff. 10.3.71. PMID 1748393. "OECD Reviews of Health Systems OECD Reviews of Health Systems: Russian Federation 2012": 38.
The smart Trick of You Should Examine All Of The Following Except That Nobody is Talking About
" Social well-being; Social security; Benefits in kind; National health plans". The brand-new Encyclopdia Britannica (15th ed.). Chicago: Encyclopdia Britannica. ISBN 978-0-85229-443-7. Obtained September 30, 2013. Richards, Raymond (1993 ). " 2 Social Security Acts". Closing the door to destitution: the shaping of the Social Security Acts of the United States and New Zealand.
p. 14. ISBN 978-0-271-02665-7. Retrieved March 11, 2013. Mein Smith, Philippa (2012 ). " Making New Zealand 19301949". A concise history of New Zealand (second ed.). Cambridge: Cambridge University Press. pp. 16465. ISBN 978-1-107-40217-1. Obtained March 11, 2013. Serner, Uncas (1980 ). "Swedish health legislation: turning points in reorganisation given that 1945". In Heidenheimer, Arnold J.; Elvander, Nils; Hultn, Charly (eds.).
New York: St. Martin's Press. p. 103. ISBN 978-0-312-71627-1. Universal and extensive medical insurance was discussed at periods all through the Second World War, and in 1946 such an expense was voted in Parliament. For monetary and other factors, its promulgation was delayed up until 1955, at which time protection was extended to consist of drugs and illness payment, too.
( September 1, 2004). " The developmental well-being state in Scandinavia: lessons to the establishing world". Geneva: United Nations Research Study Institute for Social Advancement. p. 7. Obtained March 11, 2013. Evang, Karl (1970 ). Health services in Norway. English variation by Dorothy Burton Skrdal (3rd ed.). Oslo: Norwegian Joint Committee on International Social Policy.
23. OCLC 141033. Because 2 July 1956 the entire population of Norway has been consisted of under the required health national insurance coverage program. Gannik, Dorte; Holst, Erik; Wagner, Mardsen (1976 ). "Main healthcare". The nationwide health system in Denmark. Bethesda: National Institutes of Health. pp. 4344. hdl:2027/ pur1.32754081249264. Alestalo, Matti; Uusitalo, Hannu (1987 ).
In Plants, Peter (ed.). Development to limits: the Western European welfare states considering that The second world war, Vol. 4 Appendix (run-throughs, bibliographies, tables). Berlin: Walter de Gruyter. pp. 13740. ISBN 978-3-11-011133-0. Retrieved March 11, 2013. Taylor, Malcolm G. (1990 ). "Saskatchewan treatment insurance". Insuring national health care: the Canadian experience. Chapel Hill: University of North Carolina Press.
96130. ISBN 978-0-8078-1934-0. Maioni, Antonia (1998 ). " Check out the post right here The 1960s: the political battle". Parting at the crossroads: the introduction of health insurance coverage in the United States and Canada. Princeton: Princeton University Press. pp. 12122. ISBN 978-0-691-05796-5. Retrieved September 30, 2013. Kaser, Michael (1976 ). "The USSR". Healthcare in the Soviet Union and Eastern Europe.
The Basic Principles Of How Social Connection Affects Mental Health
7% understood about International Suicide Avoidance Day (18). Proof suggests that aspects that influence preventing or postponing treatment include lack of knowledge about aspects of mental disorder and discrimination (19). Many seek to learn more about mental health problem in the mass media, consisting of motion pictures and social media networks. What they see, of course, shapes the way they think about both psychological health problem in general and private disorders.
Because psychotic breaks, suicide, and aggravating circumstances can be shown in distorted or even comical methods, the intensity of emergency scenarios involving psychological illness might not be acknowledged. Without proper information from household members, even the clients themselves may have trouble recognizing a worsening of their condition, and when they do, they might have difficulty choosing where to try to find aid.
Nevertheless, studies have actually shown that this worry is unfounded, and conversations about suicidal tendencies can even minimize signs (20, 21). The recognition that self-destructive behavior is major and that treatment looking for often requires aid makes it easier for member of the family and other caretakers to bring in patients for first aid before a fatality can take place.
Public research has actually revealed that consuming disorders and alcohol and substance abuse are frequently seen as caused and kept by the patient's own (2224). The belief that drug abuse is because of one's own choices and mindsets can affect the value and adequacy of public alcohol and drug services and treatments (24).
Such views are rarely understood as diseases, such as cancer or heart problem (23). Emergency situation situations, such as serious dependence, withdrawal syndrome, delirium, and induced psychosis may stop working to be properly dealt with due to preconception. In addition, the understanding that patients will be treated adversely can cause them or even family members to prevent seeking treatment.
It threatens to think that mental disorder treatment is inefficient, because it can lead people to overlook emergency scenarios and stop working to seek assistance for them. Another outcome of stigma is social distancing from people with mental health problem. Social distance regarding individuals with mental disorder has been measured in some circumstances (at work, amongst next-door neighbors, and in marriage) (25).
Some Of How Does Inclusion Affect Mental Health
This issue can be even more major when social distancing takes place within the family itself. Lastly, a situation may be a lot more severe: structural discrimination. Where, for example, establishing treatment sites for mental disease in distant areas, much of which are difficult to access, can give the sensation that the issue is not in your area.
As a repercussion, people with mental disorder are a lot more likely to be preyed on. Clients may associate treatment for mental disorder, whether on an outpatient basis, in medical facility wards or in intensive care, with fear, distorted beliefs and even negative memories from previous experience. Regardless of taking their medication routinely, 2550% of clients do not report advantageous modifications (26, 27) or feel that treatment as something coercive (27, 28), which often leads them to discontinue their medication (4070% of patients) (27, 29).
The very first technique includes compassion and spoken persuasion, however when life is at danger, whether the patients' or those around them, they should be purchased in, even if versus their will. Despite whether the signs remain in remission by the end of treatment, the whole procedure may be remembered with sadness, bitterness, and pity.
Nevertheless, even with voluntary admission, clients can be dealt with in a place they repent of or have contact with other clients with similar or worse conditions. Psychotropic medications can also be seen as stigmatizing, and in an emergency environment, patients are required to use them, typically at higher dosages and frequencies than in outpatient treatment.
Physical restraint, which is also connected with emergency psychiatric treatment, gets worse the stigma for patients and subsequently affects adherence to medical treatment ($130, 31). Training the healthcare teams to utilize restraint properly and just as a last hope is vital, although not all groups are prepared for this. Research study has point some problems out that contribute to preconception in health care, either directly or indirectly impacting access to care and care quality for people with psychological diseases (4).
In Brazil, psychiatrists likewise presented unfavorable ideas about individuals with schizophrenia. Negative stereotypes existed along with the belief that tolerance to side effects of psychotropic medications. Currently, being older was related to less bias (32). Lauber et al. (33) discovered that, in personal practice, psychiatrists typically stereotype individuals with psychiatric conditions and that stigmatizing actions were not different from those of the basic population (32).
How Does Isolation Affect Mental Health Fundamentals Explained
Rettenbacher et al. (35) suggested that psychotropics might be a source of preconception, reporting that almost all psychiatrists assessed Alcohol Detox thought about psychopharmacotherapy crucial, but just 71. how does academic competition affect mental illness. 4% of them followed the very same treatment if they are diagnosed with schizophrenia (32). This kind of mindset can worsen emergency situations, bearing in mind that numerous patients require uncontrolled intervention and are provided higher doses and frequencies of medication over a few hours or days.
The nature of contact in healthcare environments, especially the in the emergency situation space and the psychiatric emergency situation system, it makes professionals correspond with individuals who have extreme and chronic symptoms. This could, paradoxically, perpetuate instead of resolve stereotyped beliefs (3). What's more, the connection is normally biased due to the fundamental imbalance of power between healthcare experts and clients, which could mitigate any positive impacts of contact (3, 3638).
In psychiatric emergencies, whether treated on an outpatient basis, in an infirmary, or in emergency situation care systems, the group's experience, combined with their treatment approach, can minimize negative and stigmatizing mindsets and result in better patient assistance. Rossler ($139) reported numerous variables of the work environment that limit care quality and can eventually lead to expert burnout, counting non-supportive environments, unsupported places, restricted means, inadequate centers, and stigma towards the psychological health team.
For instance, nurses reported that bad schedule of resources and infrastructure obstructed security (areas that handle psychiatric emergencies must provide adequate protection for clients and staff), which exacerbates the insecurity of taking care of patients with mental disorder and might postpone or to avoid care (41, 42). On the other hand, professionals who look after individuals with compound usage conditions, who have better support in their services, showed more positive mindsets towards patients (40).
Other reasons for tension consist of a lack of positive feedback, bad pay, and an undesirable work environment. A client's suicide is https://www.liveinternet.ru/users/camruscarc/post476782851/ also an essential variable for many experts, and lots of report signs of post-traumatic tension after an occasion (39). Stigma can likewise affect health specialists, which might intensify public preconception as well as impact postures towards look up treatment.

(43) investigated the way psychiatrists and psychiatry are seen by different groups. Popular Drug Rehab opinion frequently has the idea that psychiatry does not produce results and can even be hazardous, which psychiatrists are low-status doctors who use too lots of psychotropic medications. The media presents psychiatry as a specialty without training, representing psychiatrists as madmen, healers, and even charlatans - how does mental illness affect physical health.
Not known Details About How Makeup Affects Your Mental Health
Mental disorder stigma, help looking for, and public health programs. Am J Public Health (2013) 103( 5 ):77780. doi: 10. 2105/AJPH.2012. 301056PubMed Abstract CrossRef Full Text Google Scholar 20. Dazzi T, Gribble R, Wessely S, Fear NT. Does inquiring about suicide and related behaviours cause self-destructive ideation? What is the evidence? Psychol Medication (2014) 44( 16 ):33613.
1017/S0033291714001299PubMed Abstract CrossRef Full Text Google Scholar 21. Oexle N, Rusch N. [Preconception - threat element and effect of suicidal habits: Ramifications for suicide avoidance] Nervenarzt (2018) 89( 7 ):77983. doi: 10. 1007/s00115 -017 -0450 -8PubMed Abstract CrossRef Complete Text Google Scholar 22. Crisp A, Gelder M, Goddard E, Meltzer H. Stigmatization of people with mental disorders: a follow-up study within the Changing Minds project of the Royal College of Psychiatrists.
PubMed Abstract Google Scholar 24. Committee on the Science of Altering Behavioral Health Social Norms, Board on Behavioral, Cognitive, and Sensory Sciences, Division of Behavioral and Social Sciences and Education, National Academies of Sciences, Engineering, and Medication. Ending Discrimination Against People with Mental and Compound Usage Disorders: The Proof for Preconception Modification.
doi: 10. 17226/23442CrossRef Full Text Google Scholar 25. Zolezzi M, Alamri M, Shaar S, Rainkie D. Preconception related to psychological illness and its treatment in the Arab culture: An organized evaluation. Int J Soc Psychiatry (2018) 64( 6 ):597609. doi: 10. 1177/0020764018789200PubMed Abstract CrossRef Full Text Google Scholar 26. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al.
N Engl J Med (2005) 353( 12 ):120923. doi: 10. 1056/NEJMoa051688PubMed Abstract CrossRef Full Text Google Scholar 27. Martinez-Hernaez A, Pie-Balaguer A, Serrano-Miguel M, Morales-Saez N, Garcia-Santesmases A, Bekele D, et al. The collaborative management of antipsychotic medication and its challenges: A qualitative study. Soc Sci Med (2020) 247:112811. doi: 10. 1016/j.
2020. 112811PubMed Abstract CrossRef Full Text Google Scholar 28. Verbeke E, Vanheule S, Cauwe J, Truijens F, Froyen B. Browbeating and power in psychiatry: A qualitative research study with ex-patients. Soc Sci Medication (2019) 223:8996. doi: 10. 1016/j. socscimed. 2019. 01 (how does social media affect mental Mental Health Delray health).031PubMed Abstract CrossRef Full Text Google Scholar 29. Tiihonen J, Mittendorfer-Rutz E, Majak M, et al.
How Does Mental Health Affect College Students Things To Know Before You Buy
JAMA Psychiatry (2017) 74( 7 ):68693. doi: 10. 1001/jamapsychiatry. 2017.1322PubMed Abstract CrossRef Complete Text Google Scholar 31. Ye J, Wang C, Xiao A, Xia Z, Yu L, Lin J, et al. Physical restraint in psychological health nursing: A concept analysis. Int J Nurs Sci (2019) 6( 3 ):3438. doi: 10. 1016/j. ijnss. 2019. 04.002PubMed Abstract CrossRef Complete Text Google Scholar 32.
O estigma atribudo pelos psiquiatras aos indivduos com esquizofrenia. Arch Clin Psychiatry (So Paulo) (2011) 38:1737. doi: 10. 1590/S0101 -60832011000500001CrossRef Complete Text Google Scholar 34. Nordt C, Rossler W, Lauber C. Mindsets of psychological health experts towards individuals with schizophrenia and significant depression. Schizophr Bull (2006) 32( 4 ):70914. doi: 10. 1093/schbul/sbj065PubMed Abstract CrossRef Complete Text Google Scholar 35.
Schizophrenia: mindsets of clients and professional carers towards the illness and antipsychotic medication. Pharmacopsychiatry (2004) 37( 3 ):1039. doi: 10. 1055/s -2004 -818987PubMed Abstract CrossRef Full Text Google Scholar 36. Bell JS, Johns R, Chen TF. Pharmacy students' and graduates' attitudes towards people with schizophrenia and serious anxiety. Am J Pharm Educ (2006) 70( 4 ):77.
5688/aj700477PubMed Abstract CrossRef Complete Text Google Scholar 37. Hinshaw SP, Cicchetti D. Stigma and mental disorder: conceptions of health problem, public mindsets, personal disclosure, and social policy. Dev Psychopathol (2000) 12( 4 ):55598. doi: 10. 1017/S0954579400004028PubMed Abstract CrossRef Complete Text Google Scholar 40. van Boekel LC, Brouwers EP, van Weeghel Addiction Treatment Delray J, Garretsen HF.
Drug Alcohol Depend (2013) 131( 1-2):2335. doi: 10. 1016/j. drugalcdep. 2013. 02.018PubMed Abstract CrossRef Full Text Google Scholar 41. Ross CA, Goldner EM. Stigma, lack of confidences and discrimination towards mental disease within the nursing profession: an evaluation of the literature. J Psychiatr Ment Health Nurs (2009) 16( 6 ):55867. doi: 10. 1111/j. 1365-2850.
xPubMed Abstract CrossRef Full Text Google Scholar 42. Bink AB. Preconception and Discrimination in Behavioral and Physical Healthcare Settings Washington, DC: The National Academies of Sciences, Engineering, and Medicine. Vol. 11. (2015 ). 43. Sartorius N, Gaebel W, Cleveland HR, Stuart H, Akiyama T, Arboleda-Florez J, et al. WPA guidance on how to fight stigmatization of psychiatry and psychiatrists.
Not known Details About How Does Eating Healthy Affect Your Mental Health
doi: 10. 1002/j. 2051-5545. 2010. tb00296. xPubMed Abstract CrossRef Complete Text Google Scholar 44. Gaebel W, Zaske H, Cleveland HR, Zielasek J, Stuart H, Arboleda-Florez J, et al. Determining the stigma of psychiatry and psychiatrists: advancement of a survey. Eur Arch Psychiatry Clin Neurosci (2011) 261( Suppl 2): S119123. doi: 10. 1007/s00406 -011 -0252 -0PubMed Abstract CrossRef Complete Text Google Scholar 45.
![]()
Dealing with minority clients with depression and anxiety: what does the evidence tell us? Gen Hosp Psychiatry (2006) 28( 1 ):2736. doi: 10. 1016/j. genhosppsych. 2005. 07.002PubMed Abstract CrossRef Full Text Google Scholar 46. Giacco D, Matanov A, Priebe S. Providing psychological healthcare to immigrants: present difficulties and new strategies. Curr Opin Psychiatry (2014) 27( 4 ):2828.
1097/YCO.0000000000000065PubMed Abstract CrossRef Full Text Google Scholar 49. Camp DL, Finlay WM, Lyons E. Is low self-confidence an unavoidable repercussion of stigma? An example from ladies with chronic psychological health issue. Soc Sci Med (2002) 55( 5 ):82334. doi: 10. 1016/S0277 -9536( 01 )00205-2PubMed Abstract CrossRef Complete Text Google Scholar 51. Sickel AE, Seacat JD, Nabors NA.
Adv Ment Health (2014) 12( 3 ):20215. doi: 10. 1080/18374905. 2014.11081898CrossRef Full Text Google Scholar 53. Tyrer P, Sharfstein S, O'Reilly R, Allison S, Bastiampillai T. Psychiatric health center beds: an Orwellian crisis. Lancet (2017) 389( 10067 ):363. doi: 10. 1016/S0140 -6736( 17 )30149-6CrossRef Complete Text Google Scholar 54. Osby U, Correia N, Brandt L, Ekbom A, Sparen P.

BMJ (2000) 321( 7259 ):4834. doi: 10. 1136/bmj. 321.7259. 483PubMed Abstract CrossRef Complete Text Google Scholar 55. Pirkola S, Sohlman B, Heila H, Wahlbeck K. Reductions in postdischarge suicide after deinstitutionalization and decentralization: a nationwide register research study in Finland. Psychiatr Serv (2007) 58( 2 ):2216. doi: 10. 1176/ps. 2007.58. 2.221PubMed Abstract CrossRef Complete Drug and Alcohol Treatment Center Text Google Scholar 56.
Effects of a psychiatric label on medical citizens' attitudes. Int J Soc Psychiatry (2012) 58( 5 ):4857. doi: 10. 1177/0020764011408652PubMed Abstract CrossRef Full Text Google Scholar 57. Gaebel W, Bauman A, Zaske H. Intervening in a multi-level network: progress of the German Open the Doors Projects. World Psychiatry (2005) 4:1620. 58. Beldie A, den Boer JA, Brain C, Constant E, Figueira ML, Filipcic I, et al.
Not known Factual Statements About How Does Bullying Affect Mental Health
Soc Psychiatry Psychiatr Epidemiol (2012) 47( Suppl 1):138. doi: 10. 1007/s00127 -012 -0491- zCrossRef Complete Text Google Scholar 59. Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rusch N. Challenging the public preconception of mental health problem: a meta-analysis of outcome research studies. Psychiatr Serv (2012) 63( 10 ):96373. doi: 10. 1176/appi. ps. 201100529PubMed Abstract CrossRef Full Text Google Scholar 61.
Brazilian standards for the management of psychomotor agitation. Part 2. Pharmacological approach. Braz J Psychiatry (2019) 41( 4 ):32435. doi: 10. 1590/1516 -4446 -2018 -0177PubMed Abstract CrossRef Complete Text Google Scholar 62. Knox DK, Holloman GH Jr. Usage and avoidance of privacy and restraint: consensus statement of the american association for emergency situation psychiatry project Beta privacy and restraint workgroup.
doi: 10. 5811/westjem. 2011.9. 6867PubMed Abstract CrossRef Complete Text Google Scholar 65. Pettigrew TF, Tropp L. Does intergroup contact lower prejudice?: Current meta-analytic findings. In: Oskamp S, editor. Minimizing prejudice and discrimination. Mahwah, NJ: LEA; (2000 ). 66. Levin S, van Laar C, Sidanius J. The effects of ingroup and outgroup relationships on ethnic attitudes in college: a longitudinal study.
The What Affects Do Violenve Have On The Mental Health Ideas
7% understood about International Suicide Avoidance Day (18). Evidence suggests that elements that influence preventing or postponing treatment include ignorance about aspects of mental disorder and discrimination (19). Numerous seek to discover mental illness in the mass media, including motion pictures and social networks. What they see, naturally, shapes the method they consider both mental disorder in general and individual conditions.


Considering that psychotic breaks, suicide, and intensifying situations can be shown in distorted or even funny methods, the severity of emergency situations including psychological illness may not be recognized. Without proper details from member of the family, even the clients themselves may have problem recognizing a worsening of their condition, and when they do, they might have trouble deciding where to search for help.
However, studies have actually shown that this worry is unfounded, and conversations about suicidal tendencies can even reduce symptoms (20, 21). The acknowledgment that self-destructive habits is major and that treatment looking for frequently requires aid makes it easier for relative and other caretakers to generate clients for first aid prior to a fatality can occur.
Public research study has shown that eating conditions and alcohol and drug abuse are frequently seen as caused and kept by the patient's own (2224). The belief that drug abuse is because of one's own choices and attitudes can influence the worth and adequacy of public alcohol and drug services and treatments (24).
Such views are rarely understood as diseases, such as cancer or cardiovascular disease (23). Emergency circumstances, such as extreme dependence, withdrawal syndrome, delirium, and induced psychosis might stop working to be properly dealt with due to stigma. In addition, the understanding that clients will be treated negatively can trigger them or perhaps household members to avoid seeking treatment.
It threatens to believe that mental disorder treatment is inefficient, because it can lead individuals to neglect emergency situation situations and fail to look for help for them. Another outcome of stigma is social distancing from individuals with psychological disease. Social distance relating to people with mental disorder has actually been determined in some situations (at work, among neighbors, and in marriage) (25).
The Best Guide To How Does Isolation Affect Mental Health
This problem can be much more severe when social distancing occurs within the family itself. Lastly, a situation may be a lot more major: structural discrimination. Where, for example, establishing treatment sites for mental disorder in far-off areas, numerous of which are tough to access, can give the sensation that the problem is not in your region.
As an effect, people with mental health problem are far more likely to be preyed on. Patients may associate treatment for psychological health problem, whether on an outpatient basis, in health center wards or in intensive care, with fear, distorted beliefs and even unfavorable memories from previous experience. In spite of taking their medication regularly, 2550% of clients do not report beneficial modifications (26, 27) or feel that treatment as something coercive (27, 28), which frequently leads them to stop their medication (4070% of clients) (27, 29).
The first approach includes empathy and verbal persuasion, however when life is at threat, whether the patients' or those around them, they need to be purchased in, even if against their will. Regardless of whether the symptoms are in remission by the end of treatment, the whole procedure may be kept in mind with sadness, bitterness, and pity.
Nevertheless, even with voluntary admission, clients can be dealt with in a place they are embarrassed of or have contact with other patients with similar or even worse conditions. Psychotropic medications can also be viewed as stigmatizing, and in an emergency environment, patients are required to use them, typically at higher doses and frequencies than in outpatient treatment.
Physical restraint, which is likewise associated with emergency situation psychiatric treatment, worsens the stigma for patients and subsequently influences adherence to medical treatment ($130, 31). Training the health care groups to utilize restraint correctly and only as a last resort is important, although not all teams are prepared for this. Research has point some concerns out that add to preconception in health care, either straight or indirectly impacting access to care and care quality for individuals with mental disorders (4).
In Brazil, psychiatrists likewise presented negative ideas about individuals with schizophrenia. Negative stereotypes existed together with the belief that tolerance to negative effects of psychotropic medications. Already, being older was related to less prejudice (32). Lauber et al. (33) found that, in personal practice, psychiatrists typically stereotype people with psychiatric disorders and that stigmatizing actions were not various from those of the general population (32).
The Definitive Guide for How Can Poor Mental Health Affect Your Physical Health
Rettenbacher et al. (35) suggested that psychotropics might be a source of stigma, reporting that nearly all psychiatrists assessed thought about psychopharmacotherapy important, but just 71. how does stresss affect our mental health. 4% of them followed the very same treatment if they are diagnosed with schizophrenia (32). This kind of attitude can intensify emergency situations, bearing in mind that many clients require uncontrolled intervention and are provided greater doses and frequencies of medication over a couple of hours or days.
The nature of contact in health care environments, especially the in the emergency clinic and the psychiatric emergency system, it makes experts communicate with people who have extreme and chronic symptoms. This could, paradoxically, perpetuate rather than eliminate stereotypical beliefs (3). What's more, the connection is normally biased due to the intrinsic imbalance of power in between healthcare specialists and clients, which might reduce any favorable results of contact https://www.liveinternet.ru/users/camruscarc/post476782851/ (3, 3638).
In psychiatric emergencies, whether dealt with on an outpatient basis, in an infirmary, or in emergency care systems, the team's experience, integrated with their treatment technique, can lower unfavorable and stigmatizing mindsets and result in much better patient support. Rossler ($139) reported several variables of the work environment that limit care quality and can eventually cause expert burnout, counting non-supportive environments, unsupported locations, limited methods, insufficient centers, and preconception towards the mental health team.
For circumstances, nurses reported that poor schedule of resources and infrastructure hindered Alcohol Detox security (places that handle psychiatric emergencies should offer sufficient security for clients and staff), which exacerbates the insecurity of taking care of clients with psychological health problem and may delay or to keep away from care (41, 42). On the Drug Rehab other hand, professionals who care for people with substance use conditions, who have much better support in their services, showed more favorable attitudes towards clients (40).
Other causes of tension consist of an absence of positive feedback, poor pay, and an undesirable workplace. A patient's suicide is also an essential variable for numerous experts, and lots of report signs of post-traumatic stress after an event (39). Preconception can likewise affect health professionals, which could worsen public stigma in addition to influence postures towards appearance up treatment.
(43) examined the way psychiatrists and psychiatry are viewed by various groups. Popular opinion often has the idea that psychiatry does not produce outcomes and can even be damaging, which psychiatrists are low-status physicians who use too lots of psychotropic medications. The media provides psychiatry as a specialized without training, representing psychiatrists as madmen, therapists, or perhaps charlatans - how does the skeletal system affect mental wellbeing.
What Does What To Do When Mental Health Affects Work Mean?
Mental disorder stigma, aid seeking, and public health programs. Am J Public Health (2013) 103( 5 ):77780. doi: 10. 2105/AJPH.2012. 301056PubMed Abstract CrossRef Complete Text Google Scholar 20. Dazzi T, Gribble R, Wessely S, Fear NT. Does inquiring about suicide and related behaviours cause suicidal ideation? What is the evidence? Psychol Medication (2014) 44( 16 ):33613.
1017/S0033291714001299PubMed Abstract CrossRef Full Text Google Scholar 21. Oexle N, Rusch N. [Stigma - danger element and repercussion of suicidal behavior: Implications for suicide prevention] Nervenarzt (2018) 89( 7 ):77983. doi: 10. 1007/s00115 -017 -0450 -8PubMed Abstract CrossRef Complete Text Google Scholar 22. Crisp A, Gelder M, Goddard E, Meltzer H. Stigmatization of people with mental disorders: a follow-up research study within the Changing Minds project of the Royal College of Psychiatrists.
PubMed Abstract Google Scholar 24. Committee on the Science of Changing Behavioral Health Social Norms, Board on Behavioral, Cognitive, and Sensory Sciences, Department of Behavioral and Social Sciences and Education, National Academies of Sciences, Engineering, and Medicine. Ending Discrimination Versus Individuals with Psychological and Substance Usage Disorders: The Proof for Stigma Change.
doi: 10. 17226/23442CrossRef Full Text Google Scholar 25. Zolezzi M, Alamri M, Shaar S, Rainkie D. Preconception related to mental disorder and its treatment in the Arab Drug and Alcohol Treatment Center culture: An organized evaluation. Int J Soc Psychiatry (2018) 64( 6 ):597609. doi: 10. 1177/0020764018789200PubMed Abstract CrossRef Full Text Google Scholar 26. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al.
N Engl J Med (2005) 353( 12 ):120923. doi: 10. 1056/NEJMoa051688PubMed Abstract CrossRef Complete Text Google Scholar 27. Martinez-Hernaez A, Pie-Balaguer A, Serrano-Miguel M, Morales-Saez N, Garcia-Santesmases A, Bekele D, et al. The collective management of antipsychotic medication and its barriers: A qualitative research study. Soc Sci Medication (2020) 247:112811. doi: 10. 1016/j.
2020. 112811PubMed Abstract CrossRef Full Text Google Scholar 28. Verbeke E, Vanheule S, Cauwe J, Truijens F, Froyen B. Browbeating and power in psychiatry: A qualitative study with ex-patients. Soc Sci Med (2019) 223:8996. doi: 10. 1016/j. socscimed. 2019. 01 (how does substance abuse affect your mental health).031PubMed Abstract CrossRef Complete Text Google Scholar 29. Tiihonen J, Mittendorfer-Rutz E, Majak M, et al.
Getting The How Does Physical Activity Affect Mental Health To Work
JAMA Psychiatry (2017) 74( 7 ):68693. doi: 10. 1001/jamapsychiatry. 2017.1322PubMed Abstract CrossRef Complete Text Google Scholar 31. Ye J, Wang C, Xiao A, Xia Z, Yu L, Lin J, et al. Physical restraint in mental health nursing: A concept analysis. Int J Nurs Sci (2019) 6( 3 ):3438. doi: 10. 1016/j. ijnss. 2019. 04.002PubMed Abstract CrossRef Full Text Google Scholar 32.
O estigma atribudo pelos psiquiatras aos indivduos com esquizofrenia. Arch Clin Psychiatry (So Paulo) (2011) 38:1737. doi: 10. 1590/S0101 -60832011000500001CrossRef Full Text Google Scholar 34. Nordt C, Rossler W, Lauber C. Attitudes of psychological health professionals toward individuals with schizophrenia and major anxiety. Schizophr Bull (2006) 32( 4 ):70914. doi: 10. 1093/schbul/sbj065PubMed Abstract CrossRef Complete Text Google Scholar 35.
Schizophrenia: mindsets of clients and expert carers towards the disease and antipsychotic medication. Pharmacopsychiatry (2004) 37( 3 ):1039. doi: 10. 1055/s -2004 -818987PubMed Abstract CrossRef Complete Text Google Scholar 36. Bell JS, Johns R, Chen TF. Pharmacy trainees' and graduates' mindsets towards people with schizophrenia and extreme depression. Am J Pharm Educ (2006) 70( 4 ):77.
5688/aj700477PubMed Abstract CrossRef Complete Text Google Scholar 37. Hinshaw SP, Cicchetti D. Stigma and mental illness: conceptions of health problem, public attitudes, individual disclosure, and social policy. Dev Psychopathol (2000) 12( 4 ):55598. doi: 10. 1017/S0954579400004028PubMed Abstract CrossRef Complete Text Google Scholar 40. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF.
Drug Alcohol Depend (2013) 131( 1-2):2335. doi: 10. 1016/j. drugalcdep. 2013. 02.018PubMed Abstract CrossRef Complete Text Google Scholar 41. Ross CA, Goldner EM. Preconception, negative mindsets and discrimination towards psychological health problem within the nursing profession: a review of the literature. J Psychiatr Ment Health Nurs (2009) 16( 6 ):55867. doi: 10. 1111/j. 1365-2850.
xPubMed Abstract CrossRef Complete Text Google Scholar 42. Bink AB. Preconception and Discrimination in Behavioral and Physical Healthcare Settings Washington, DC: The National Academies of Sciences, Engineering, and Medicine. Vol. 11. (2015 ). 43. Sartorius N, Gaebel W, Cleveland HR, Stuart H, Akiyama T, Arboleda-Florez J, et al. WPA guidance on how to fight stigmatization of psychiatry and psychiatrists.
What Are Drugs That Can Affect Your Mental Health - An Overview
doi: 10. 1002/j. 2051-5545. 2010. tb00296. xPubMed Abstract CrossRef Full Text Google Scholar 44. Gaebel W, Zaske H, Cleveland HR, Zielasek J, Stuart H, Arboleda-Florez J, et al. Determining the preconception of psychiatry and psychiatrists: development of a survey. Eur Arch Psychiatry Clin Neurosci (2011) 261( Suppl 2): S119123. doi: 10. 1007/s00406 -011 -0252 -0PubMed Abstract CrossRef Full Text Google Scholar 45.
Treating minority clients with anxiety and stress and anxiety: what does the evidence tell us? Gen Hosp Psychiatry (2006) 28( 1 ):2736. doi: 10. 1016/j. genhosppsych. 2005. 07.002PubMed Abstract CrossRef Complete Text Google Scholar 46. Giacco D, Matanov A, Priebe S. Providing mental health care to immigrants: current difficulties and brand-new strategies. Curr Opin Psychiatry (2014) 27( Addiction Treatment Delray 4 ):2828.
1097/YCO.0000000000000065PubMed Abstract CrossRef Complete Text Google Scholar 49. Camp DL, Finlay WM, Lyons E. Is low self-confidence an inescapable repercussion of stigma? An example from women with persistent mental illness. Soc Sci Med (2002) 55( 5 ):82334. doi: 10. 1016/S0277 -9536( 01 )00205-2PubMed Abstract CrossRef Complete Text Google Scholar 51. Sickel AE, Seacat JD, Nabors NA.
Adv Ment Health (2014) 12( 3 ):20215. doi: 10. 1080/18374905. 2014.11081898CrossRef Full Text Google Scholar 53. Tyrer P, Sharfstein S, O'Reilly R, Allison S, Bastiampillai T. Psychiatric medical facility beds: an Orwellian crisis. Lancet (2017) 389( 10067 ):363. doi: 10. 1016/S0140 -6736( 17 )30149-6CrossRef Complete Text Google Scholar 54. Osby U, Correia N, Brandt L, Ekbom A, Sparen P.
BMJ (2000) 321( 7259 ):4834. doi: 10. 1136/bmj. 321.7259. 483PubMed Abstract CrossRef Full Text Google Scholar 55. Pirkola S, Sohlman B, Heila H, Wahlbeck K. Reductions in postdischarge suicide after deinstitutionalization and decentralization: an across the country register research study in Finland. Psychiatr Serv (2007) 58( 2 ):2216. doi: 10. 1176/ps. 2007.58. 2.221PubMed Abstract CrossRef Complete Text Google Scholar 56.
Impacts of a psychiatric label on medical homeowners' attitudes. Int J Soc Mental Health Delray Psychiatry (2012) 58( 5 ):4857. doi: 10. 1177/0020764011408652PubMed Abstract CrossRef Complete Text Google Scholar 57. Gaebel W, Bauman A, Zaske H. Intervening in a multi-level network: development of the German Open the Doors Projects. World Psychiatry (2005) 4:1620. 58. Beldie A, den Boer JA, Brain C, Constant E, Figueira ML, Filipcic I, et al.
The Main Principles Of What Are The Factors That Affect Mental And Emotional Health

Soc Psychiatry Psychiatr Epidemiol (2012) 47( Suppl 1):138. doi: 10. 1007/s00127 -012 -0491- zCrossRef Complete Text Google Scholar 59. Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rusch N. Challenging the public preconception of psychological illness: a meta-analysis of result research studies. Psychiatr Serv (2012) 63( 10 ):96373. doi: 10. 1176/appi. ps. 201100529PubMed Abstract CrossRef Full Text Google Scholar 61.
Brazilian guidelines for the management of psychomotor agitation. Part 2. Pharmacological method. Braz J Psychiatry (2019) 41( 4 ):32435. doi: 10. 1590/1516 -4446 -2018 -0177PubMed Abstract CrossRef Full Text Google Scholar 62. Knox DK, Holloman GH Jr. Usage and avoidance of seclusion and restraint: agreement statement of the american association for emergency psychiatry task Beta privacy and restraint workgroup.

doi: 10. 5811/westjem. 2011.9. 6867PubMed Abstract CrossRef Complete Text Google Scholar 65. Pettigrew TF, Tropp L. Does intergroup contact decrease prejudice?: Current meta-analytic findings. In: Oskamp S, editor. Lowering prejudice and discrimination. Mahwah, NJ: LEA; (2000 ). 66. Levin S, van Laar C, Sidanius J. The results of ingroup and outgroup friendships on ethnic attitudes in college: a longitudinal study.
Little Known Facts About What Affects Can Mental Health And Health And Wellbeing Have On Career.
7% learnt about International Suicide Avoidance Day (18). Proof suggests that elements that influence avoiding or delaying treatment consist of ignorance about aspects of mental disorder and discrimination (19). Many seek to learn about mental disorder in the mass media, consisting of films and social media networks. What they see, obviously, shapes the way they consider both mental illness in general and individual disorders.
Given that psychotic breaks, suicide, and aggravating scenarios can be shown in distorted or even comical methods, the severity of emergency situation situations including psychological health problem might not be recognized. Without appropriate info from member of the family, even the clients themselves may have trouble recognizing a worsening of their condition, and when they do, they might have difficulty choosing where to search for aid.
Nevertheless, research studies have shown that this fear is unproven, and conversations about suicidal tendencies can even reduce signs (20, 21). The acknowledgment that self-destructive behavior is major which treatment looking for often requires help makes it much easier for household members and other caretakers to bring in clients for emergency treatment prior to a death can occur.
Public research has shown that consuming conditions and alcohol and drug abuse are often seen as triggered and preserved by the patient's own (2224). The belief that substance abuse is because of one's own choices and attitudes can affect the value and adequacy of public alcohol and drug services and treatments (24).
Such views are rarely understood as illness, such as cancer or heart illness (23). Emergency circumstances, such as serious reliance, withdrawal syndrome, delirium, and induced psychosis may stop working to be correctly addressed due to preconception. In addition, the understanding that patients will be dealt with negatively can cause them or perhaps relative to prevent looking for treatment.
It is hazardous to think that psychological illness treatment is inefficient, since it can lead individuals to overlook emergency circumstances and stop working to look for help for them. Another result of stigma is social distancing from people with mental disorder. Social distance regarding individuals with mental illness has been measured in some circumstances (at work, amongst next-door neighbors, and in marital relationship) (25).

The Basic Principles Of How Can Poor Mental Health Affect Your Physical Health
This issue can be much more major when social distancing takes place within the household itself. Finally, a circumstance may be much more severe: structural discrimination. Where, for instance, establishing treatment sites for mental disorder in remote areas, a lot of which are challenging to Alcohol Detox access, can offer the feeling that the issue is not in your area.
As a consequence, individuals with mental disorder are far more likely to be preyed on. Patients might associate treatment for mental disease, whether on an outpatient basis, in health center wards or in extensive care, with worry, distorted beliefs and even unfavorable memories from previous experience. In spite of taking their medication frequently, 2550% of clients do not report useful changes (26, 27) or feel that treatment as something coercive (27, 28), which typically leads them to cease their medication (4070% of patients) (27, 29).
The very first technique includes empathy and spoken persuasion, but when life is at risk, whether the clients' or those around them, they must be purchased in, even if versus their will. No matter whether the signs remain in remission by the end of treatment, the entire procedure may be kept in mind with sadness, bitterness, and shame.
However, even with voluntary admission, clients can be dealt with in a place they are ashamed of or have contact with other clients with similar or even worse conditions. Psychotropic medications can also be viewed as stigmatizing, and in an emergency environment, clients are required to utilize them, frequently at higher doses and frequencies than in outpatient treatment.

Physical restraint, which is likewise associated with emergency psychiatric treatment, gets worse the preconception for clients and consequently affects adherence to medical treatment ($130, 31). Training the health care groups to use restraint properly and only as a last hope is necessary, although not all groups are prepared for this. Research has point some concerns out that contribute to preconception in healthcare, either directly or indirectly impacting access to care and care quality for people with mental illnesses (4).
In Brazil, psychiatrists also provided negative ideas about people with schizophrenia. Unfavorable stereotypes were present along with the belief that tolerance to adverse effects of psychotropic medications. Currently, being older was associated with less bias (32). Lauber et al. (33) discovered that, in private practice, psychiatrists typically stereotype individuals with psychiatric conditions which stigmatizing actions were not various from those of the basic population (32).
Some Known Details About Drug Rehab Why Does Mental Health Affect Physical Health
Rettenbacher et al. (35) recommended that psychotropics might be a source of stigma, reporting that almost all psychiatrists examined thought about psychopharmacotherapy essential, but just 71. how does mental illness affect physical health. 4% of them followed the same treatment if they are detected with schizophrenia (32). This kind of attitude can exacerbate emergency situations, keeping in mind that lots of clients need involuntary intervention and are provided greater doses and frequencies of medication over a couple of hours or days.
The nature of contact in healthcare environments, specifically the in the emergency room and the psychiatric emergency unit, it makes experts communicate with individuals who have serious and chronic signs. This could, paradoxically, perpetuate rather than dispel stereotyped beliefs (3). What's more, the connection is typically biased due to the inherent imbalance of power in between healthcare specialists and clients, which could mitigate any favorable effects of contact (3, 3638).
In psychiatric emergencies, whether dealt with on an outpatient basis, in an infirmary, or in emergency care systems, the group's experience, integrated with their treatment method, https://www.liveinternet.ru/users/camruscarc/post476782851/ can decrease unfavorable and stigmatizing attitudes and result in much better patient support. Rossler ($139) reported a number of variables of the workplace that limit care quality and can eventually result in expert burnout, counting non-supportive environments, unsupported areas, restricted means, insufficient centers, and preconception towards the mental health team.
For instance, nurses reported that bad accessibility of resources and infrastructure hindered security (areas that handle psychiatric emergency situations should offer sufficient security for patients and staff), which worsens the insecurity of looking after clients with psychological illness and may delay or to avoid care (41, 42). On the other hand, professionals who care for individuals with substance use conditions, who have better support in their services, showed more favorable mindsets towards clients (40).
Other reasons for stress include an absence of favorable feedback, poor pay, and an undesirable workplace. A patient's suicide is also an essential variable for numerous specialists, and many report signs of post-traumatic tension after an occasion (39). Stigma can also affect health specialists, which could exacerbate public preconception as well as influence postures toward look up treatment.
(43) investigated the method psychiatrists and psychiatry are viewed by various groups. Public viewpoint frequently has the concept that psychiatry does not produce outcomes and can even be harmful, and that psychiatrists are low-status doctors who use a lot of psychotropic medications. The media presents psychiatry as a specialized without training, representing psychiatrists as madmen, therapists, and even charlatans - how does body image affect mental health.
The Facts About How Makeup Affects Your Mental Health Revealed
More than half of people with mental disorder don't look for assistance for their conditions. Typically, people avoid or delay looking for treatment due to concerns about being treated in a different way or fears of losing their jobs and livelihood. That's since preconception, bias and discrimination against people with mental disorder is still quite a problem.
People with psychological disease are marginalized and victimized in various methods, however comprehending what that appears like and how to address and eradicate it can assist. Preconception typically originates from lack of understanding or worry. Inaccurate or misleading media representations of mental disorder contribute to both those elements. An evaluation of research studies on preconception programs that while the general public may accept the medical or hereditary nature of a psychological health disorder and the need for treatment, lots of individuals still have a negative view of those with mental disorder.
refers to the lack of confidences, including internalized shame, that individuals with mental health problem have about their own condition., is more systemic, including policies of federal government and personal organizations that deliberately or accidentally limitation opportunities for people with mental disorder. Examples consist of lower funding for psychological disease research study or fewer psychological health services relative to other healthcare. $193. 2 billion in lost incomes every year. 90% of those who died by suicide had a hidden mental illness. Individuals with mental disorders live next door, teach our kids, operate in the next cubicle, and being in the very same seat at church. If we show these individuals respect and approval, we help remove one of the barriers to them effectively coping with their diseases.
Find out the realities rather of the misconceptions. Supporter within your circles of impact to make sure these people have the very same rights and opportunities as everybody else. Typically the daily things, like having people see you as a specific not a disease, make the greatest difference. After preconception, another major barrier to getting treatment is cost.

How Does Mental Illness Affect Society Things To Know https://telegra.ph/some-known-details-about-how-meth-affects-your-mental-health-11-07 Before You Get This
The variety of people we can help each year depends upon the generosity of our donors. In 2017, the PAF assisted around 2,500 people. Jean Holthaus, LMSW, LISW has been providing outpatient treatment services since 1995 when she earned her Masters of Social Work degree from the University of Iowa.
She presently acts as supervisor of the Telehealth Center and the Hastings Clinic and is likewise a Pine Rest Outpatient Regional Director (how does sleep affect mental health).
Stigma is when somebody sees you in a negative method since of a specific characteristic or attribute (such as skin colour, cultural background, an impairment or a mental disorder). When somebody treats you in an unfavorable method since of your mental disease, this is discrimination. Preconception happens when an individual defines someone by their disease instead of who they are as an individual.
For people with mental health problems, the social preconception and discrimination they experience can make their issues worse, making it harder to recover. It may trigger the individual to avoid getting the assistance they require since of the fear of being stigmatised. Some of the effects of stigma consist of: feelings of pity, hopelessness and isolation reluctance to request aid or to get treatment absence of understanding by household, good friends or others fewer chances for work or social interaction bullying, View website physical violence or harassment self-doubt the belief that you will never conquer your illness or have the ability to accomplish what you desire in life.
The 20-Second Trick For How Do Mental Disorders Affect Rational Thought
Attempt not to let the worry of being labelled with a mental disorder stop you from getting aid. Sometimes, if you hear or experience something typically enough, you start to think it yourself. Try not to let other individuals's ignorance influence the method you feel about yourself (how does stresss affect our mental health). Psychological disease is not a sign of weakness and is hardly ever something you can deal with by yourself.
Lots of individuals with mental disorder wish to separate themselves from the world. Reaching out to individuals you trust family, good friends, coaches or religious leaders can mean you get the support you require. Joining a psychological health support system either online or face to face can help you deal with sensations of seclusion and make you realise that you are not alone in your sensations and experiences.
Instead of saying 'I'm schizophrenic', say 'I have schizophrenia'. There is power in language. Bear in mind that other individuals's judgements typically originate from a lack of understanding rather than anything else. These judgments are made before they are familiar with you, so do not think that their views have anything to do with you personally.
The Victorian Equal Opportunity and Person Rights Commission promotes level playing field and can help you attend to unlawful discrimination. The Australian Human Rights Commission is a Commonwealth Federal government company that promotes human rights and handle compliance and discrimination. At the international level, the United Nations General Assembly has 'Principles for the security of individuals with mental disorder and the enhancement of mental health care'.
How Does Tv Affect A Child Mental Development for Dummies
Everybody has a role to play in creating a mentally healthy neighborhood one that is inclusive, turns down discrimination and supports recovery. Ways to help include: finding out the truths about mental illness and sharing them with family, good friends, work colleagues and classmates learning more about people Substance Abuse Treatment with personal experiences of mental disorder so you find out to see them for the individual they are rather than their disease.
Deal with all people with regard and self-respect. preventing using language that puts the disease first and the person second. Say 'a person with bipolar affective disorder' rather than 'that individual is bipolar'. stating something when you hear people around you making stereotypical or inaccurate comments about psychological illness. sharing your own experience of mental health problem (if you have actually experienced it).
Mental disorder is not something disgraceful that requires to be hidden. This page has actually been produced in assessment with and approved by: Better Health Channel - (require new cp) Content on this site is supplied for information purposes only. Details about a treatment, service, item or treatment does not in any method endorse or support such treatment, service, item or treatment and is not intended to replace advice from your medical professional or other authorized health professional.
Get This Report on How Physical Health Affects Mental Health
More than half of people with mental disorder do not look for assistance for their conditions. Typically, individuals prevent or delay seeking treatment due to issues about being dealt with differently or fears of losing their tasks and livelihood. That's due to the fact that stigma, bias and discrimination versus people with psychological illness is still quite a problem.
Individuals with mental health problem are marginalized and victimized in different methods, but understanding what that looks like and how to attend to and eliminate it can help. Stigma often originates from lack of understanding or fear. Inaccurate or View website deceptive media representations of mental disease contribute to both those elements. An evaluation of studies on stigma programs that while the public might accept the medical or hereditary nature of a psychological health condition and the need for treatment, lots of people still have an unfavorable view of those with psychological illness.
refers to the unfavorable mindsets, including internalized shame, that people with mental disorder have about their own condition., is more systemic, including policies of federal government and personal companies that deliberately or unintentionally limit chances for people with psychological disease. Examples include lower financing for mental disorder research study or less mental health services relative to other health care. $193. 2 billion in lost profits every year. 90% of those who died by suicide had a hidden mental disorder. Individuals with mental disorders live next door, teach our children, work in the next cubicle, and being in the same seat at church. If we reveal these individuals respect and approval, Substance Abuse Treatment we help remove one of the barriers to them effectively managing their illnesses.
Discover the facts instead of the misconceptions. Supporter within your circles of impact to make sure these people have the same rights and chances as everyone else. Typically the daily things, like having people see you as a private not an illness, make the most significant distinction. After preconception, another major barrier to getting treatment is expense.
The smart Trick of How Does Inclusion Affect Mental Health That Nobody is Discussing
The number of individuals we can assist each year depends upon the generosity of our donors. In 2017, the PAF helped around 2,500 people. Jean Holthaus, LMSW, LISW has been offering outpatient treatment services because 1995 when she made her Masters of Social Work degree from the University of Iowa.
She currently works as manager of the Telehealth Clinic and the Hastings Center and is also a Pine Rest Outpatient Regional Director (how does culture affect mental health).
Preconception is when somebody sees you in a negative way because of a specific characteristic or quality (such as skin colour, cultural background, a special needs or a psychological illness). When someone treats you in an unfavorable way because of your mental disorder, this is discrimination. Preconception takes place when an individual specifies someone by their disease rather than who they are as an individual.
For people with psychological health problems, https://telegra.ph/some-known-details-about-how-meth-affects-your-mental-health-11-07 the social preconception and discrimination they experience can make their problems worse, making it more difficult to recuperate. It may cause the individual to avoid getting the help they need because of the worry of being stigmatised. A few of the effects of stigma consist of: sensations of pity, hopelessness and isolation reluctance to request for help or to get treatment lack of understanding by household, friends or others fewer opportunities for work or social interaction bullying, physical violence or harassment insecurity the belief that you will never overcome your disease or be able to achieve what you want in life.
Some Known Details About How Does Mental Illness Affect High School Students
Attempt not to let the fear of being labelled with a mental health problem stop you from getting help. In some cases, if you hear or experience something typically enough, you begin to believe it yourself. Try not to let other individuals's ignorance influence the way you feel about yourself (how does mental illness affect work). Psychological illness is not an indication of weak point and is hardly ever something you can handle on your own.
Many people with mental disorder wish to separate themselves from the world. Connecting to individuals you trust household, friends, coaches or spiritual leaders can suggest you get the support you require. Signing up with a psychological health support group either online or personally can help you deal with feelings of seclusion and make you realise that you are not alone in your feelings and experiences.
Rather of stating 'I'm schizophrenic', say 'I have schizophrenia'. There is power in language. Keep in mind that other individuals's judgements frequently originate from an absence of understanding instead of anything else. These judgments are made before they are familiar with you, so do not believe that their views have anything to do with you personally.
The Victorian Equal Opportunity and Human being Rights Commission promotes equal opportunity and can help you resolve unlawful discrimination. The Australian Human Rights Commission is a Commonwealth Government agency that promotes human rights and handle compliance and discrimination. At the global level, the United Nations General Assembly has 'Principles for the defense of individuals with mental disease and the improvement of mental healthcare'.
Not known Facts About How Does Mental Health Affect School
Everyone has a function to play in developing a psychologically healthy neighborhood one that is inclusive, turns down discrimination and supports healing. Ways to help include: finding out the realities about mental health problem and sharing them with family, good friends, work associates and classmates being familiar with individuals with personal experiences of mental disorder so you find out to see them for the individual they are instead of their health problem.
Deal with all people with regard and self-respect. avoiding utilizing language that puts the illness first and the individual 2nd. State 'a person with bipolar affective disorder' instead of 'that individual is bipolar'. stating something when you hear people around you making stereotypical or inaccurate remarks about psychological illness. sharing your own experience of mental disorder (if you have experienced it).

Mental disorder is not something shameful that requires to be concealed. This page has actually been produced in consultation with and authorized by: Better Health Channel - (require brand-new cp) Material on this website is attended to info functions just. Info about a treatment, service, product or treatment does not in any way endorse or support such treatment, service, product or treatment and is not meant to change advice from your doctor or other authorized health specialist.
Getting My How To Get Someone Admitted To A Mental Health Facility To Work
The bottom line: purchasing a psychologically healthy labor force benefits business. 16 million Americans impacted by depression every year 50% Of individuals with depression are untreated $44 billion The cost to employers of work environment anxiety 40-60% Decrease in absenteeism and presenteeism with treatment $1 Of financial investment in treatment for anxiety and anxiety results in a return of $4 in better health and work performance. how teaching affects your mental health.
We understand that back-to-work plans often fail to supply the support that individuals with mental illness need to stay well, go back to, or begin work. Getting the best support can make a big difference to your psychological health, so that's why we're campaigning to alter these plans. You can learn more about our back-to-work project and how to get included by learning more about our back-to-work manifesto.
For much of us, work is a major part of our lives. It is where we spend much of our time, where we get our earnings and typically where we make our buddies. Having a satisfying job can be helpful for your mental health and general wellbeing. All of us have times when life gets on top people in some cases that's job-related, like due dates or travel.
The value contributed to the economy by individuals who are at work and have actually or have actually had mental health problems is as high as $1225 billion each year, which represents 12.1% of the UK's overall GDP. It's crucial that we safeguard that value by resolving psychological health at work for those with existing concerns, for those at risk, and for the workforce as a whole.
The smart Trick of How Stigma Affects Mental Health And Substance Use Treatment That Nobody is Discussing
Our company believe in work environments where everybody can grow. We also think in the role of companies, workers and businesses in producing flourishing communities. Excellent psychological health at work and excellent management go together and there is strong evidence that offices with high levels of psychological wellness are more efficient.
After reading this guide you ought to: Mental health is the way we think and feel and our ability to deal with ups and downs. Psychological health is something we all have. When we take pleasure in great mental health, we have a sense of purpose and instructions, the energy to do the things we wish to do, and the capability to deal with the obstacles that happen in our lives.
Mental health is simply the very same. If you take pleasure in great mental health, you can: maximize your potential handle what life throws at you play a full part in your relationships, your workplace, and your neighborhood. Your mental health does not always stay the very same. It can change as scenarios change and as you move through different phases in your life.
It could be something in the house, the pressure of work, or the start of a mental illness like anxiety. When we feel distressed, we require a compassionate, human response. The earlier website we have the ability http://shanepsck881.cavandoragh.org/top-guidelines-of-how-to-get-a-mental-health-evaluation to acknowledge when something isn't quite best, the earlier we can get assistance. We all have times when we feel down, stressed or frightened.
The 6-Second Trick For How Mental Health Affects The Environment
For some people, psychological health issue become complex, and require support and treatment for life. Aspects like hardship, genetics, childhood trauma, discrimination, or continuous physical disease make it more most likely that we will develop psychological health issues, but psychological illness can occur to anyone. Our research shows that many people have some experience of a mental health issue, and the current massive survey in England suggested that one in six people experience the symptoms of a mental illness in any offered week.
Various mental health issues impact individuals in different ways and it's essential to understand a person's experience. Medical diagnosis is not a guaranteed way to understand an individual's experience. Some individuals with schizophrenia for example live practically regular lives, and some people with stress and anxiety are significantly affected by their condition.
Mental illness can have a great deal of various signs and signs. As a guideline, you must look for aid from your GP if you have hard feelings that are: stopping you from proceeding with life having a huge effect on individuals you live or work with affecting your state of mind over a number of weeks triggering you to have ideas of suicide.
We might make uncharacteristic errors, find it difficult to inspire ourselves, our timekeeping might slip, or we may be short tempered. We might look or feel extremely exhausted or drained. We might find we isolate ourselves, avoid colleagues or appear distracted. We might hesitate more or grind to a stop entirely.
The Only Guide for How Mental Health Affects Presidents
We might discover these early indication difficult to see in ourselves, and it can assist to have associates who can assist us connect this to our psychological health. If things development, you may see more obvious indications of a mental illness in a colleague outbursts of anger or feeling, lacks from work, or not looking after their appearance as they usually would.
Awareness of psychological health is increasing, but we still face a world where people with psychological illness deal with discrimination, and can face difficulties getting the help they require. Numerous individuals who experience distress try to keep their feelings concealed since they hesitate of other people's actions. Worry of discrimination and sensations of pity are amongst the top factors people provide for not informing their coworkers about their psychological health problems.
However, the choice to disclose distress at work is not one people ignore. It is vital Click for more info that offices end up being environments where individuals feel safe to be themselves. We have a large variety of legal rights that protect our mental health at work. These variety from fundamental human rights such as the right to liberty of expression and liberty of association, to the health and safety legislation that keeps us safe from dangers, including mental hazards.

This indicates that individuals with mental health issues are secured from discrimination and harassment and are entitled to reasonable changes to adjust their task or work. To be thought about disabled under equality legislation, a person should have a disability that has "a significant, adverse, and long-term influence on their ability to bring out everyday jobs". The Equality Commission for Northern Ireland provides details about the different protections for individuals with psychological health problems in Northern Ireland.
The Definitive Guide to How The Environment Affects Mental Health
A modification is intended to level the playing field by getting rid of a barrier to the task that is offered by the effect of their psychological illness. Examples of reasonable modifications: Changing a person's working pattern to allow them to begin later on or end up earlier since of the side impacts of medication, or permitting them to take a trip the night prior to meetings and remain over to avoid morning travel. how self-esteem affects mental health.
Excusing somebody from attending work functions and client events including food, rather enabling them to establish alternative networking plans that attain comparable service returns. Access to Work is a government-funded scheme that can assist to fund devices, software application, and other support if expense is a barrier to making affordable modifications.
Little Known Questions About What Do Mental Health Counselors Do.
The bottom line: purchasing a psychologically healthy labor force is excellent for company. 16 million Americans impacted by anxiety every year 50% Of individuals with anxiety are neglected $44 billion The expense to employers of Click for more info work environment anxiety 40-60% Decrease in absence and presenteeism with treatment $1 Of financial investment in treatment for depression and anxiety leads to a return of $4 in much better health and work efficiency. how sleep affects mental health.
We understand that back-to-work plans typically fail to offer the support that people with psychological health issue need to stay well, go back to, or begin work. Getting the best support can make a huge difference to your psychological health, so that's why we're campaigning to alter these plans. You can learn more about our back-to-work campaign and how to get involved by learning more about our back-to-work manifesto.
For a lot of us, work is a huge part of our lives. It is where we invest much of our time, where we get our income and frequently where we make our good friends. Having a satisfying job can be great for your psychological health and basic wellbeing. All of us have times when life gets on top people in some cases that's job-related, like due dates or travel.
The worth contributed to the economy by individuals who are at work and have or have had psychological health issue is as high as $1225 billion per year, which represents 12.1% of the UK's total GDP. It's essential that we protect that value by attending to mental health at work for those with existing problems, for those at danger, and for the workforce as a whole.
How A Patient Body Language Affects Doctors Mental Health Things To Know Before You Buy
Our company believe in work environments where everybody can grow. We also think in the role of employers, staff members and organizations in producing thriving neighborhoods. Good psychological health at work and excellent management go together and there is strong proof that work environments with high levels of mental wellness are more productive.
After reading this guide you need to: Psychological health is the way we think and feel and our capability to handle ups and downs. Mental health is something all of us have. When we enjoy good psychological health, we have a sense of purpose and instructions, the energy to do the important things we wish to do, and the capability to deal with the obstacles that happen in our lives.

Psychological health is simply the very same. If you enjoy excellent mental health, you can: maximize your potential cope with what life throws at you play a full part in your relationships, your work environment, and your neighborhood. Your psychological health does not always remain the same. It can change as circumstances change and as you move through various stages in your life.
It could be something in your home, the pressure of work, or the start of a psychological health issue like depression. When we feel distressed, we need a caring, human response. The earlier we have the ability to recognise when something isn't quite best, the earlier we can get assistance. We all have times when we feel down, stressed or scared.
The Ultimate Guide To How Diet Affects Mental Health
For some people, psychological health problems end up being complex, and require assistance and treatment for life. Aspects like poverty, genes, childhood trauma, discrimination, or ongoing physical illness make it most likely that we will develop psychological health problems, however psychological illness can occur to any person. Our research study reveals that many people have some experience of a mental health issue, and the newest massive survey in England suggested that a person in 6 individuals experience the symptoms of a psychological illness in any offered week.
Different psychological health issue affect individuals in different ways and it's essential to comprehend a person's experience. Medical diagnosis is not a guaranteed way to understand a person's experience. Some individuals with schizophrenia for example live practically ordinary lives, and some individuals with anxiety are severely impacted by their condition.
Psychological health issue can have a lot of different signs and indications. As a guideline, you need to look for aid from your GP if you have hard feelings that are: stopping you from getting on with life having a big effect on the people you live or work with impacting your mood over several weeks triggering you to have thoughts of suicide.
We may make uncharacteristic errors, discover it difficult to encourage ourselves, our timekeeping might slip, or we might be brief tempered. We might look or feel extremely exhausted or drained pipes. We might discover we isolate ourselves, prevent coworkers or appear sidetracked. We may hesitate more or grind to a stop altogether.
Top Guidelines Of How Social Media Affects Mental Health Essay
We might find these early indication hard to see in ourselves, and it website can assist to have coworkers who can help us link this to our psychological health. If things progress, you might see more obvious indications of a mental health issue in a colleague outbursts of anger or feeling, absences from work, or not taking care of their appearance as they normally would.
Awareness of psychological health is increasing, but we still face a world where individuals with mental health issue face discrimination, and can face challenges getting the help they require. Lots of people who experience distress try to keep their sensations hidden due to the fact that they hesitate of other individuals's reactions. Worry of discrimination and sensations of embarassment are among the leading factors individuals give for not informing their colleagues about their psychological illness.
Even so, the decision to reveal distress at work is not one people ignore. It is important that offices become environments where people feel safe to be themselves. We have a wide variety of legal rights that protect our psychological health at work. These variety from standard human rights such as the right to flexibility of expression and flexibility of association, to the health and wellness legislation that keeps us safe from hazards, consisting of mental hazards.
This implies that people with psychological illness are safeguarded from discrimination and harassment and are entitled to affordable modifications to adapt their job or work. To be thought about disabled under equality legislation, an individual should have a problems that has "a considerable, unfavorable, and long-term influence on their ability to perform daily tasks". The Equality Commission for Northern Ireland provides details about the different defenses for individuals with mental illness in Northern Ireland.
Not known Details About Why Mental Health Affects Every Thing I Do
An adjustment http://shanepsck881.cavandoragh.org/top-guidelines-of-how-to-get-a-mental-health-evaluation is intended to level the playing field by eliminating a barrier to the task that is supplied by the impact of their psychological illness. Examples of sensible adjustments: Altering an individual's working pattern to allow them to begin later or end up earlier due to the fact that of the negative effects of medication, or allowing them to travel the night before conferences and stay over to avoid morning travel. how dating at a young age affects mental health.
Excusing someone from attending work functions and customer events involving food, instead enabling them to establish alternative networking plans that accomplish similar business returns. Access to Work is a government-funded plan that can assist to fund devices, software, and other assistance if cost is a barrier to making reasonable adjustments.
